Month: August 2024
C-Section Recovery: Comparing the After Effects of Emergency and Planned Procedures

Childbirth is a life-changing event filled with anticipation and excitement, but it can also come with its challenges. For some mothers, a Cesarean section (C-section) is necessary to ensure the safety of both mother and baby. C-sections can be categorized into two types: emergency and planned (or elective). Each type of procedure has unique implications for recovery. In this article, we’ll explore the after effects of emergency C-sections compared to planned C-sections, shedding light on what mothers can expect during their recovery journeys.
Understanding C-Sections: Emergency vs. Planned
What is a C-Section?
A Cesarean section is a surgical procedure used to deliver a baby through incisions made in the mother’s abdomen and uterus. While many women opt for vaginal births, some require C-sections for various medical reasons, including:
– Emergency C-Section: This is performed when complications arise during labor or delivery, such as fetal distress, placenta previa, or uterine rupture. In such cases, the surgery is urgent to ensure the safety of both mother and baby.
– Planned C-Section: Also known as an elective C-section, this procedure is scheduled in advance. Reasons for choosing a planned C-section may include previous C-sections, certain medical conditions, or concerns about the baby’s size.
Recovery Process Overview
Regardless of the type of C-section, recovery is an essential part of the birthing process. However, the experiences and challenges faced by mothers may differ based on whether the C-section was emergency or planned.
Immediate After Effects
1. Surgical Recovery Time
Emergency C-Section: Mothers undergoing emergency C-sections may experience a longer initial recovery time due to the nature of the surgery. The urgency of the situation can lead to additional complications, such as increased blood loss or infections. As a result, recovery may be more challenging, requiring a longer stay in the hospital.
Planned C-Section: Women who have a planned C-section often have a smoother recovery process. Since the procedure is scheduled, there is typically less urgency, and the surgical team can take their time to minimize complications. Many mothers report feeling more prepared for the procedure, which can positively influence their recovery experience.
2. Pain Management
Emergency C-Section: Pain management can be more complex following an emergency C-section. The mother may have been in labor for some time before the surgery, leading to exhaustion and heightened pain sensitivity. Additionally, if complications arise, pain management may be more intensive, requiring stronger medications.
Planned C-Section: In contrast, women undergoing planned C-sections often have a more predictable pain management regimen. Since the procedure is anticipated, the healthcare team can plan for adequate pain relief from the outset. Mothers may also feel more in control of their pain management choices, which can lead to a more positive recovery experience.
3. Emotional Well-Being
Emergency C-Section: The experience of an emergency C-section can be emotionally taxing. Mothers may feel a sense of loss or disappointment if their birth plan included a vaginal delivery. Additionally, unexpected complications can lead to feelings of anxiety or trauma. It’s essential for healthcare providers to address the emotional needs of these mothers as part of their recovery.
Planned C-Section: Mothers undergoing a planned C-section often feel more emotionally prepared for the experience. Having the opportunity to discuss the procedure, ask questions, and set expectations can reduce anxiety. However, some mothers may still experience mixed feelings about not having a vaginal delivery.
Long-Term After Effects
1. Physical Recovery and Complications
Emergency C-Section: The recovery period following an emergency C-section can be more complicated due to potential surgical complications. Women may face risks such as:
– Infection: A higher likelihood of developing an infection at the incision site.
– Blood Clots: Increased risk of blood clots due to prolonged immobility.
– Scarring: More extensive scarring if the surgery was performed under stressful circumstances.
Planned C-Section: While complications can still arise during a planned C-section, the risk may be lower due to better surgical conditions. Mothers are typically more informed about the recovery process, allowing them to take proactive steps to minimize risks, such as:
– Following post-operative care instructions.
– Engaging in gentle physical activity as advised.
– Attending follow-up appointments to monitor healing.
2. Breastfeeding Challenges
Emergency C-Section: Breastfeeding may present challenges for mothers who have had an emergency C-section. Pain, fatigue, and the impact of anesthesia can make it difficult for these mothers to initiate breastfeeding promptly. Additionally, if the baby requires additional medical attention, it may delay skin-to-skin contact and breastfeeding.
Planned C-Section: In a planned C-section, healthcare providers often implement practices to support breastfeeding immediately after delivery. This can include encouraging skin-to-skin contact as soon as the mother is stable. Many mothers find it easier to establish breastfeeding when they are prepared for the procedure and have received support from the medical team.
3. Long-Term Physical Impact
Emergency C-Section: Some women may experience longer-term physical effects following an emergency C-section, including:
– Chronic Pain: Some may develop chronic pain in the abdominal area due to nerve damage or scar tissue.
– Adhesions: Internal scar tissue can lead to adhesions, which may cause pain or complications in future pregnancies.
Planned C-Section: While planned C-sections also carry the risk of chronic pain and adhesions, many women report better overall recovery experiences. The planned nature of the procedure allows for better surgical techniques and follow-up care.
Emotional and Psychological Considerations
1. Impact of Birth Experience
Emergency C-Section: The experience of an emergency C-section can leave lasting emotional scars for some mothers. Feelings of helplessness or fear during the surgery may contribute to post-traumatic stress disorder (PTSD) or other emotional challenges. It’s crucial for these mothers to receive emotional support from healthcare providers, family, and friends.
Planned C-Section: While many mothers who have planned C-sections report feeling more in control, they may still experience complex emotions. It’s essential to acknowledge that every birth experience is unique, and mothers may have varied feelings about their delivery method.
2. Support Systems
Emergency C-Section: Mothers recovering from emergency C-sections may benefit from strong support systems. Encouragement from partners, family, and friends can help alleviate stress and facilitate healing. Counseling or support groups can also provide a safe space for mothers to share their experiences.
Planned C-Section: Support systems are equally important for mothers who have had planned C-sections. Being able to share their birth stories, whether positive or negative, can aid in emotional recovery. Engaging in discussions with other mothers who have had similar experiences can also provide valuable insights.
Recovering from a C-section, whether emergency or planned, is a unique journey that requires patience, understanding, and support. Both types of C-sections come with distinct after effects that can influence physical recovery, emotional well-being, and overall experiences. By acknowledging these differences and addressing the unique needs of mothers, we can foster a supportive environment that promotes healing and empowerment.
As each mother’s experience is personal
How to Plan a Kids’ Birthday Party: Who to Invite and Why It Matters

Planning a kid’s birthday party is an exciting yet sometimes daunting task. From choosing the theme to arranging the activities, there are many decisions to make. But one of the most significant—and often challenging—decisions is figuring out who to invite. Creating the guest list can be tricky, especially when you want to make sure your child has a fantastic time without causing unintentional hurt feelings or social dilemmas. In this article, we'll explore the importance of the guest list, offer tips on who to invite, and share strategies to ensure that everyone has a great time.
Why the Guest List Matters
The guest list is one of the most important elements of planning a birthday party because it sets the tone for the entire event. The right mix of guests can create a fun, inclusive atmosphere where everyone feels welcome and your child has a blast. On the other hand, a poorly considered guest list can lead to awkward situations, conflicts, or even hurt feelings—both for your child and the guests.
Choosing who to invite also helps you plan other aspects of the party, such as the venue, the number of activities, and the amount of food you'll need. It’s essential to consider the size of the space you’re working with and the nature of the activities planned. For instance, a small, intimate gathering might be perfect for a home party, while a larger group might require renting a venue with more space.
Consider Your Child’s Wishes
Before you start creating the guest list, have a conversation with your child. Ask them who they would like to invite and why. This discussion can provide valuable insights into your child’s social circle and who their close friends are. Some kids might have a clear idea of who they want at their party, while others may need a little guidance.
If your child is younger, they might not fully understand the implications of excluding someone, so you may need to step in and suggest inviting a broader range of classmates or friends to avoid hurt feelings. On the other hand, older children might be more aware of social dynamics and could have specific preferences. Either way, it’s essential to respect your child’s choices while also considering the feelings of others.
The Size of the Party
The size of the party will largely dictate who to invite. If you’re planning a small gathering, you may need to be more selective with the guest list. This might mean inviting just a few close friends or family members. For larger parties, you can extend invitations to a broader group, such as the entire class or neighborhood kids.
When deciding on the size of the party, consider the following factors:
– Venue Capacity: How many people can comfortably fit in the chosen location?
– Budget:How much can you afford to spend per guest? Larger parties generally require more resources.
– Activities: Are the planned activities better suited for a small group or a large crowd?
A good rule of thumb is to match the number of guests to your child’s age—so a 7-year-old might have seven guests, an 8-year-old eight guests, and so on. However, this isn’t a hard and fast rule, and you should adjust based on what feels right for your child and your circumstances.
Family First?
When creating your guest list, you might wonder whether you should invite family members—particularly if your child is close to cousins or other relatives around the same age. Family can be a natural choice for the guest list, especially if your child has a strong bond with them. However, it’s also important to ensure that your child’s friends are included. A good balance is key; too many family members can turn the party into a family reunion rather than a celebration with your child’s peers.
If you’re planning to invite extended family, consider organizing a separate family gathering, especially if your child wants their school friends to have more focus at the main party. This way, your child gets to enjoy time with both groups without feeling overwhelmed.
Navigating School Politics
Inviting classmates can be one of the trickiest aspects of planning a birthday party. There’s often a fine line between including everyone and keeping the party manageable. Here are some strategies to help navigate school politics:
1. The “Invite the Whole Class” Approach
One way to avoid hurt feelings is to invite the entire class. This ensures that no one feels left out and can foster a sense of inclusivity. However, inviting the whole class can be expensive and logistically challenging, especially if you’re hosting the party at home.
If you’re going this route, consider hosting the party at a venue that’s equipped to handle large groups, such as a park, community center, or rented party space. Many venues offer packages for large groups that include food, activities, and decorations, which can help streamline the planning process.
2. Gender-Specific Parties
Some parents opt to host gender-specific parties, inviting only boys or girls. While this can make planning easier and limit the guest list, it’s essential to ensure that your child’s closest friends are included, regardless of gender.
3. Small Groups
If inviting the entire class isn’t feasible, another option is to invite a smaller, more intimate group of friends. To avoid hurt feelings, it’s best to keep the invitations discreet. You can send them directly to the parents or distribute them outside of school hours.
Encourage your child to choose friends they genuinely enjoy spending time with, rather than feeling obligated to invite everyone. This approach can lead to a more meaningful and enjoyable experience for your child and their guests.
Sibling Dilemmas
When planning a birthday party, you’ll also need to consider whether to invite siblings of the invited guests. This can be a tricky situation—some parents may assume that siblings are automatically invited, while others may not. To avoid confusion, it’s best to be clear in your invitations.
If you’re hosting a small party and space is limited, it’s perfectly acceptable to politely specify that the invitation is only for the invited child. You can do this by mentioning in the invitation that the party is for “[Your Child’s Name] and their friends,” or by stating the number of guests you’re expecting.
On the other hand, if you have plenty of space and resources, inviting siblings can make things easier for parents, as they won’t have to arrange separate childcare. Just be sure to account for the additional guests when planning activities, food, and party favors.
How to Handle RSVPs
Once the invitations are sent out, managing RSVPs is crucial to ensuring you’re adequately prepared. Request that parents RSVP by a specific date, and consider following up with those who haven’t responded.
Be prepared for last-minute changes—some guests may cancel at the last minute, while others might show up without RSVPing. It’s always a good idea to have a little extra food and a few additional party favors on hand, just in case.
If you’re hosting the party at a venue with a strict guest limit, communicate this clearly in the invitation and when following up on RSVPs. This way, parents understand the importance of confirming their child’s attendance.
Making Everyone Feel Included
Once the guest list is finalized, it’s essential to ensure that everyone feels included and has a good time. Here are some tips to make the party enjoyable for all guests:
– Plan Inclusive Activities: Choose games and activities that are suitable for the entire group. Avoid activities that might single out or exclude certain children. Group games, crafts, or team activities are great for fostering a sense of inclusion.
– Create a Welcoming Environment: Make sure the party atmosphere is warm and welcoming. Greet each child as they arrive, and encourage your child to include everyone in the activities. If there are children who are shy or don’t know the other guests well, help them feel comfortable by introducing them to others or pairing them with a buddy.
– Party Favors for Everyone: Ensure that each guest leaves with a party favor, regardless of how long they stayed at the party or whether they participated in every activity. This helps every child feel appreciated and part of the celebration.
Dealing with Uninvited Guests
Despite your best efforts, you may encounter situations where uninvited guests show up. Whether it’s an extra sibling or a child who assumed they were invited, handling these situations with grace is key.
If space allows, try to include the uninvited guest without making a big deal out of it. The goal is to avoid causing any discomfort or hurt feelings. If it’s not possible to accommodate the extra guest due to space or safety concerns, a polite and understanding explanation to the parent can help manage the situation.
Planning a kids' birthday party and deciding who to invite can be a balancing act. However, with thoughtful consideration, clear communication, and a focus on inclusivity, you can create a guest list that ensures a fun, memorable celebration for your child and their friends.
Remember that the guest list should reflect your child’s wishes, the size of the venue, and your ability to host a certain number of guests. By keeping these factors in mind, you’ll be well on your way to throwing a birthday party that’s not only enjoyable for your child but also creates wonderful memories for all who attend.
Why Some Parents Choose to Say No to the Hep B Shot for Newborns: What You Need to Know

As a new parent, one of the many decisions you’ll face is whether to vaccinate your newborn. One of the first vaccines offered is the Hepatitis B (Hep B) shot, typically administered within 24 hours of birth. However, some parents are hesitant or choose to delay or decline this vaccine for their newborns. This article explores the reasons behind this decision, the benefits and risks of the Hep B vaccine, and what you should consider when making an informed choice for your child.
Understanding Hepatitis B
Hepatitis B is a viral infection that affects the liver. It is transmitted through contact with infected blood and other bodily fluids, such as through unprotected sex, sharing needles, or from an infected mother to her baby during childbirth. The infection can be acute (short-term) or chronic (long-term). Chronic Hepatitis B can lead to serious health problems, including liver damage, cirrhosis, liver cancer, and death.
The Hep B vaccine is designed to protect against this infection. It’s a series of shots given over several months, with the first dose typically administered at birth.
Why the Hep B Vaccine is Recommended for Newborns
The Centers for Disease Control and Prevention (CDC) and the American Academy of Pediatrics (AAP) recommend that all newborns receive the Hep B vaccine within 24 hours of birth. This recommendation is based on several factors:
1. Early Protection: Administering the Hep B vaccine at birth provides early protection against Hepatitis B, especially for babies born to mothers who are infected with the virus. Even if a mother tests negative, there is still a small risk of infection from other sources.
2. Prevention of Chronic Hepatitis B: Infants who contract Hepatitis B are more likely to develop chronic infections, which can lead to severe liver disease later in life. Early vaccination significantly reduces this risk.
3. High Safety Profile: The Hep B vaccine has been extensively studied and is considered safe and effective. Side effects are generally mild, such as a sore arm or low-grade fever.
Reasons Some Parents Choose to Decline the Hep B Vaccine
Despite these recommendations, some parents opt to say no to the Hep B shot for their newborns. The decision to delay or decline the vaccine is often based on a variety of personal beliefs, concerns, and considerations.
1. Perception of Low Risk
One of the most common reasons parents choose to decline the Hep B vaccine at birth is the belief that their newborn is not at high risk of contracting the virus. They may feel that since Hepatitis B is primarily transmitted through sexual contact, needle sharing, or from an infected mother, their baby is unlikely to be exposed to the virus in early life. Parents who test negative for Hepatitis B may also feel that their child is not immediately at risk.
While this reasoning is understandable, it’s important to note that Hepatitis B can be contracted in various ways, and the virus can survive outside the body for at least seven days. Accidental exposure, such as through minor cuts or contact with infected blood, is possible, though rare.
2. Concerns About Vaccine Ingredients
Some parents express concerns about the ingredients used in vaccines, including the Hep B shot. These concerns often revolve around the use of aluminum as an adjuvant, which helps enhance the body’s immune response to the vaccine.
Aluminum is naturally found in the environment and is present in small amounts in many foods and water. The amount of aluminum in vaccines is considered safe by health organizations, including the CDC and the World Health Organization (WHO). However, some parents worry about the cumulative effects of aluminum exposure, particularly in newborns, and prefer to delay the vaccine until their child is older.
3. Desire for a Delayed Vaccine Schedule
Another reason some parents choose to decline the Hep B vaccine at birth is a preference for a delayed vaccine schedule. These parents may believe that spreading out vaccinations over a longer period is safer or that it allows their child’s immune system more time to develop before receiving multiple vaccines.
It’s important to note that delaying vaccines can leave infants vulnerable to preventable diseases during their most vulnerable early months. However, for parents who are uncomfortable with the standard vaccination schedule, discussing a customized plan with a healthcare provider is an option.
4. Misinformation and Vaccine Hesitancy
In the age of the internet, there is a vast amount of information—and misinformation—available about vaccines. Some parents are influenced by anti-vaccine rhetoric, which often includes unfounded claims about the risks of vaccines, including links to autism or other health issues. These claims have been thoroughly debunked by extensive scientific research, but they continue to contribute to vaccine hesitancy among some parents.
It’s essential to critically evaluate the sources of information and seek advice from trusted healthcare professionals when making decisions about vaccinations.
Weighing the Risks and Benefits
When deciding whether to vaccinate your newborn against Hepatitis B, it’s crucial to weigh the potential risks and benefits.
Benefits of the Hep B Vaccine
– Protection Against a Serious Disease: The most significant benefit of the Hep B vaccine is protection against Hepatitis B, a potentially life-threatening illness. Vaccination reduces the risk of chronic Hepatitis B and its associated complications, such as liver cancer and cirrhosis.
– Herd Immunity: Vaccinating your child contributes to herd immunity, which protects vulnerable individuals who cannot be vaccinated, such as those with compromised immune systems or certain medical conditions.
– Peace of Mind: Knowing that your child is protected against a dangerous virus can provide peace of mind, especially as they grow older and become more exposed to different environments and activities.
Potential Risks and Considerations
– Adverse Reactions: Like all vaccines, the Hep B shot can cause side effects. However, these are usually mild and temporary, such as soreness at the injection site or a slight fever. Serious allergic reactions are rare.
– Overwhelming the Immune System: Some parents worry that giving multiple vaccines at once, including the Hep B shot at birth, may overwhelm their baby’s immune system. However, research shows that the immune system can handle multiple vaccines simultaneously without being compromised.
– Personal Beliefs and Values: For some parents, the decision to decline or delay the Hep B vaccine is rooted in personal or cultural beliefs. It’s important to have an open dialogue with your healthcare provider about these beliefs to ensure that your concerns are addressed and that you have accurate information.
Making an Informed Decision
Deciding whether to give your newborn the Hep B vaccine is a personal choice that should be made after careful consideration of the available information and a discussion with your healthcare provider. Here are some steps to help guide your decision:
1. Educate Yourself
Take the time to learn about Hepatitis B, the Hep B vaccine, and the potential risks and benefits. Use reputable sources such as the CDC, WHO, and your healthcare provider to gather accurate and up-to-date information.
2. Discuss Your Concerns
If you have concerns about the vaccine, don’t hesitate to discuss them with your healthcare provider. They can provide evidence-based information, address your specific worries, and help you understand the implications of delaying or declining the vaccine.
3. Consider Your Baby’s Health and Risk Factors
Assess your baby’s risk of exposure to Hepatitis B based on your health, lifestyle, and environment. While the risk may seem low in the early months, consider the long-term benefits of early vaccination.
4. Weigh the Pros and Cons
Consider both the benefits of protecting your baby against a potentially severe disease and the risks associated with delaying or declining the vaccine. Make a decision that aligns with your values and your baby’s best interests.
5. Be Open to Re-Evaluating Your Decision
It’s okay to change your mind. If you initially choose to decline the Hep B shot at birth, you can always revisit the decision as your baby grows.
the time to learn about Hepatitis B, the Hep B vaccine, and the potential risks and benefits. Use reputable sources such as the CDC, WHO, and your healthcare provider to gather accurate and up-to-date information.
2. Discuss Your Concerns
If you have concerns about the vaccine, don’t hesitate to discuss them with your healthcare provider. They can provide evidence-based information, address your specific worries, and help you understand the implications of delaying or declining the vaccine.
3. Consider Your Baby’s Health and Risk Factors
Assess your baby’s risk of exposure to Hepatitis B based on your health, lifestyle, and environment. While the risk may seem low in the early months, consider the long-term benefits of early vaccination.
4. Weigh the Pros and Cons
Consider both the benefits of protecting your baby against a potentially severe disease and the risks associated with delaying or declining the vaccine. Make a decision that aligns with your values and your baby’s best interests.
5. Be Open to Re-Evaluating Your Decision
It’s okay to change your mind. If you initially choose to decline the Hep B shot at birth, you can always revisit the decision as your baby grows.
The Rising Prevalence of PCOS: Causes, Symptoms, and Treatment Options

Polycystic Ovary Syndrome (PCOS) has become an increasingly common health issue affecting women of reproductive age. This hormonal disorder, characterized by irregular menstrual cycles, excess androgen levels, and polycystic ovaries, impacts millions of women worldwide. As awareness of PCOS grows, so does the recognition of its rising prevalence, making it essential to understand the causes, symptoms, and treatment options available.
Understanding PCOS
PCOS is a complex condition that can manifest in a variety of ways, often making it difficult to diagnose. The exact cause of PCOS is still unknown, but it is believed to be linked to a combination of genetic and environmental factors. Women with PCOS often experience hormonal imbalances, particularly an excess of androgens (male hormones like testosterone), which can disrupt ovulation and lead to the development of multiple small cysts on the ovaries.
The Rise in PCOS Cases
Over the past few decades, there has been a noticeable increase in the number of women diagnosed with PCOS. While some of this rise can be attributed to improved diagnostic criteria and greater awareness among healthcare providers and patients, other factors may also be contributing to the growing prevalence of this condition.
1. Lifestyle Factors
Modern lifestyles have significantly changed in recent years, with sedentary behaviors and poor dietary habits becoming more common. High-calorie diets, rich in processed foods and sugars, combined with reduced physical activity, have led to a rise in obesity rates—a known risk factor for PCOS. Obesity can exacerbate insulin resistance, which is closely linked to PCOS. Insulin resistance causes the body to produce more insulin, which in turn can increase androgen production and worsen PCOS symptoms.
2. Environmental Influences
Exposure to certain environmental toxins, such as endocrine-disrupting chemicals (EDCs), has also been implicated in the rise of PCOS cases. EDCs are found in various products, including plastics, pesticides, and personal care items, and can interfere with hormone regulation. While more research is needed to fully understand the impact of these chemicals on PCOS development, it is a growing area of concern.
3. Genetic Predisposition
Genetics play a significant role in the development of PCOS. Women with a family history of the condition are more likely to develop it themselves. As awareness of PCOS increases, more women are being diagnosed, leading to a greater understanding of its hereditary nature. However, genetics alone do not account for the rise in PCOS, suggesting that environmental and lifestyle factors also play a crucial role.
Common Symptoms of PCOS
PCOS can present a wide range of symptoms, which can vary in severity from woman to woman. Recognizing these symptoms early on is essential for managing the condition effectively. Common symptoms of PCOS include:
1. Irregular Menstrual Cycles
One of the hallmark symptoms of PCOS is irregular or absent menstrual periods. Women with PCOS may experience fewer than nine periods a year, prolonged menstrual cycles, or heavy bleeding during periods.
2. Excess Androgen Levels
High levels of androgens can lead to physical symptoms such as excessive hair growth (hirsutism) on the face, chest, and back, as well as acne and male-pattern baldness. These symptoms can be distressing and impact a woman’s self-esteem.
3. Polycystic Ovaries
An ultrasound may reveal enlarged ovaries with multiple small cysts, a characteristic feature of PCOS. However, not all women with PCOS have polycystic ovaries, and not all women with polycystic ovaries have PCOS.
4. Weight Gain
Many women with PCOS struggle with weight gain, particularly around the abdomen. This weight gain can be challenging to manage and may contribute to insulin resistance, exacerbating PCOS symptoms.
5. Infertility
PCOS is one of the leading causes of infertility in women. The hormonal imbalances associated with PCOS can interfere with ovulation, making it difficult to conceive. However, with appropriate treatment, many women with PCOS can successfully become pregnant.
6. Mood Disorders
PCOS is often associated with mood disorders such as depression and anxiety. The emotional and psychological impact of living with a chronic condition like PCOS, combined with the physical symptoms, can contribute to mental health challenges.
Diagnosing PCOS
Diagnosing PCOS can be challenging due to its varied presentation. There is no single test for PCOS; instead, doctors typically use a combination of medical history, physical exams, blood tests, and ultrasound to diagnose the condition. The diagnostic criteria for PCOS usually include at least two of the following:
1. Irregular or absent menstrual periods.
2. Excess androgen levels, as indicated by symptoms or blood tests.**
3. Polycystic ovaries, as seen on ultrasound.
Treatment Options for PCOS
While there is no cure for PCOS, there are several treatment options available to help manage symptoms and reduce the risk of long-term health complications. Treatment plans are typically tailored to the individual’s specific symptoms and health goals.
1. Lifestyle Modifications
One of the most effective ways to manage PCOS symptoms is through lifestyle changes. Maintaining a healthy diet and regular exercise can help reduce insulin resistance, promote weight loss, and regulate menstrual cycles. Even a modest weight loss of 5-10% can significantly improve symptoms in women with PCOS.
A balanced diet rich in whole grains, fruits, vegetables, lean proteins, and healthy fats can help manage blood sugar levels and reduce inflammation. Regular physical activity, such as aerobic exercises and strength training, can also help improve insulin sensitivity and support weight management.
2. Medications
Several medications are available to help manage the symptoms of PCOS. Commonly prescribed medications include:
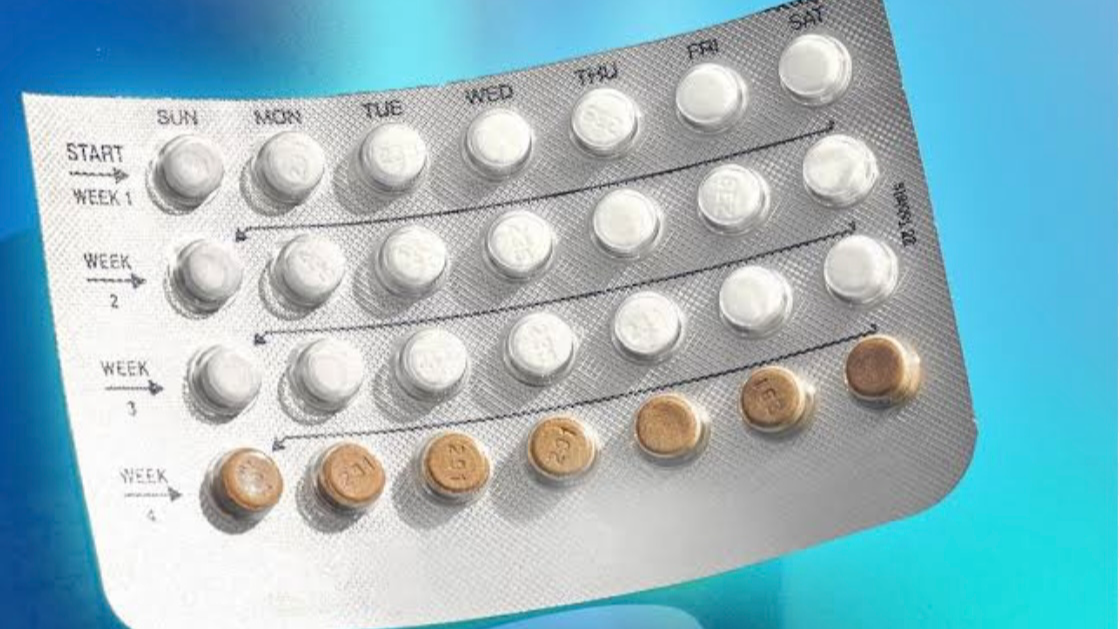
– Hormonal Birth Control: Birth control pills, patches, or vaginal rings can help regulate menstrual cycles, reduce androgen levels, and control symptoms like acne and excess hair growth.
– Metformin: This medication, commonly used to treat type 2 diabetes, can help improve insulin resistance in women with PCOS, which may regulate menstrual cycles and promote ovulation.
– Anti-Androgen Medications: These medications can help reduce androgen levels and minimize symptoms like excessive hair growth and acne.
– Fertility Medications: For women trying to conceive, fertility medications such as clomiphene or letrozole can stimulate ovulation.
3. Fertility Treatments
For women with PCOS who are struggling with infertility, various fertility treatments are available. These include ovulation induction with medications, intrauterine insemination (IUI), and in vitro fertilization (IVF). Working closely with a fertility specialist can help determine the best course of action based on individual needs and circumstances.
4. Mental Health Support
Living with PCOS can take a toll on mental health. Seeking support from a therapist or counselor can help address the emotional challenges associated with the condition. Joining support groups, either in person or online, can also provide a sense of community and understanding.
Long-Term Health Risks Associated with PCOS
PCOS is not just a reproductive issue; it can have long-term health implications if not managed properly. Women with PCOS are at an increased risk of developing several chronic conditions, including:
– Type 2 Diabetes: Insulin resistance associated with PCOS increases the risk of developing type 2 diabetes.
– Cardiovascular Disease: Women with PCOS are more likely to have high blood pressure, high cholesterol, and other risk factors for heart disease.
– Endometrial Cancer: Irregular menstrual cycles and prolonged periods without ovulation can increase the risk of endometrial cancer.
– Sleep Apnea: Obesity and insulin resistance can contribute to the development of sleep apnea, a condition characterized by interrupted breathing during sleep.
The rising prevalence of PCOS is a concerning trend that highlights the need for greater awareness and understanding of this condition. While the exact causes of the increase in PCOS cases are still being studied, it is clear that lifestyle, environmental, and genetic factors all play a role. Recognizing the symptoms of PCOS early and seeking appropriate treatment can help women manage the condition and reduce the risk of long-term health complications.
If you suspect you may have PCOS or are experiencing any of the symptoms mentioned, it’s important to consult with a healthcare provider for a proper diagnosis and personalized treatment plan. With the right support and management strategies, women with PCOS can lead healthy and fulfilling lives.
My first Post

Hi there!, This is my first post on Sistapedia….I'm interested in you!
“Should You Take Birth Control Pills for Menopausal Symptom Relief? Pros and Cons Explained”
Menopause marks a significant transition in a woman’s life, bringing with it a range of physical and emotional changes. For many, the symptoms associated with this stage—such as hot flashes, night sweats, mood swings, and irregular periods—can be overwhelming. Seeking relief from these symptoms, some women turn to various treatments, including birth control pills. But is this a good option? In this article, we'll explore the pros and cons of using birth control pills to alleviate menopausal symptoms, helping you make an informed decision.
Understanding Menopause and Perimenopause
Before diving into whether birth control pills are a viable option, it's important to understand what menopause and perimenopause entail.
Menopause is defined as the point when a woman hasn't had a menstrual period for 12 consecutive months, marking the end of her reproductive years. This typically occurs between the ages of 45 and 55, though it can happen earlier or later.
Perimenopause is the transitional phase leading up to menopause. During this time, which can last anywhere from a few months to several years, hormone levels fluctuate, leading to symptoms like irregular periods, hot flashes, and mood swings. For many women, perimenopause is the most challenging phase due to the unpredictability and intensity of these symptoms.
How Birth Control Pills Work
Birth control pills are a form of hormonal contraception that contains synthetic forms of the hormones estrogen and progesterone. They work by regulating hormone levels to prevent ovulation, thereby preventing pregnancy. However, the hormone regulation they provide can also help manage some of the symptoms associated with perimenopause.
The Potential Benefits of Birth Control Pills During Perimenopause
For some women, birth control pills can offer several benefits during perimenopause:
1. Regulation of Menstrual Cycles: One of the most frustrating symptoms of perimenopause is irregular periods. Some women may experience heavy bleeding, prolonged periods, or spotting between cycles. Birth control pills can help regulate the menstrual cycle, making periods more predictable and manageable.
2. Reduction in Hot Flashes and Night Sweats: Hot flashes and night sweats are among the most common and bothersome symptoms of perimenopause. Birth control pills, particularly those containing both estrogen and progestin, can help reduce the frequency and severity of these symptoms by stabilizing hormone levels.
3. Improvement in Mood Stability: Hormonal fluctuations during perimenopause can lead to mood swings, anxiety, and depression. Some women find that birth control pills help stabilize their mood by maintaining more consistent hormone levels.
4. Clearer Skin: Hormonal changes during perimenopause can lead to acne and other skin issues. The hormonal regulation provided by birth control pills can improve skin health for some women.
5. Bone Health: Estrogen plays a crucial role in maintaining bone density. During perimenopause, when estrogen levels begin to drop, women are at increased risk for osteoporosis. Birth control pills that contain estrogen can help protect against bone loss during this transition.
The Potential Risks and Downsides of Using Birth Control Pills During Perimenopause
While there are benefits to using birth control pills during perimenopause, there are also risks and downsides to consider:
1. Not Suitable for All Women: Birth control pills may not be appropriate for women with certain health conditions, such as a history of blood clots, breast cancer, or uncontrolled high blood pressure. It's important to discuss your medical history with your healthcare provider before starting any hormonal treatment.
2. Increased Risk of Blood Clots: Birth control pills, especially those containing estrogen, can increase the risk of blood clots. This risk is higher in women over the age of 35, particularly those who smoke or have a history of clotting disorders.
3. Potential Side Effects: Some women may experience side effects from birth control pills, such as nausea, headaches, weight gain, or changes in libido. While these side effects are often mild and temporary, they can be bothersome for some women.
4. Does Not Address All Menopausal Symptoms: While birth control pills can help manage some symptoms of perimenopause, they may not be effective for others. For example, they won't alleviate vaginal dryness, which is a common symptom as estrogen levels decline. For these symptoms, other treatments, such as vaginal estrogen creams, may be necessary.
5. Not a Long-Term Solution: Birth control pills are typically only used during perimenopause and are not recommended once menopause is reached. After menopause, hormone replacement therapy (HRT) is usually a more appropriate option for managing symptoms.
Birth Control Pills vs. Hormone Replacement Therapy (HRT)
As women transition from perimenopause to menopause, they may need to switch from birth control pills to hormone replacement therapy (HRT). While both treatments involve hormones, they serve different purposes and are tailored to different stages of a woman’s life.
Birth Control Pills: Primarily used during perimenopause to regulate menstrual cycles and alleviate symptoms related to hormonal fluctuations.
Hormone Replacement Therapy (HRT): Typically used after menopause to replace the hormones that the body no longer produces, helping to manage symptoms like hot flashes, night sweats, and vaginal dryness, and to protect bone health.
HRT usually involves lower doses of hormones compared to birth control pills and is designed to address the specific needs of postmenopausal women. However, like birth control pills, HRT also carries risks, including an increased risk of certain types of cancer, cardiovascular disease, and stroke. The decision to use HRT should be made in consultation with your healthcare provider, considering your individual health profile and symptoms.
Making an Informed Decision
Deciding whether to use birth control pills during perimenopause is a personal choice that should be made based on a careful consideration of the potential benefits and risks. Here are some steps you can take to make an informed decision:
1. Consult with Your Healthcare Provider: Your doctor can help you weigh the pros and cons of using birth control pills based on your medical history, symptoms, and overall health. They can also discuss alternative treatments if birth control pills are not suitable for you.
2. Consider Your Symptoms:If your perimenopausal symptoms are mild, you may not need to take birth control pills. On the other hand, if your symptoms are significantly affecting your quality of life, birth control pills may offer relief.
3. Evaluate Your Health Risks: If you have risk factors for blood clots, heart disease, or other health conditions, your doctor may advise against using birth control pills. Be honest about your medical history and any concerns you have.
4. Explore Alternatives :If birth control pills aren't right for you, there are other options available to manage perimenopausal symptoms. These include lifestyle changes, natural remedies, and other medications, such as low-dose antidepressants or anti-seizure medications that can help with hot flashes.
5. Monitor Your Symptoms: If you decide to use birth control pills, keep track of your symptoms and any side effects. Regular check-ups with your doctor are important to ensure that the treatment is working effectively and safely.
Using birth control pills to alleviate menopausal symptoms can be an effective option for some women, particularly during the perimenopausal phase. These pills can help regulate menstrual cycles, reduce hot flashes, and improve mood stability. However, they are not without risks and are not suitable for everyone.
The decision to use birth control pills during perimenopause should be made in consultation with your healthcare provider, taking into account your individual health needs and risks. By carefully weighing the pros and cons, you can make an informed decision that helps you navigate this important transition with greater comfort and confidence.
Remember, menopause is a natural part of aging, and while it can bring challenges, there are many ways to manage symptoms and maintain a high quality of life during this time. Whether through birth control pills, HRT, or other treatments, finding the right solution for you is key to feeling your best during and after this transition.
“Understanding AMH and Its Impact on Fertility: Key Insights for Your Reproductive Health”

When it comes to reproductive health and fertility, understanding the role of hormones is crucial. Anti-Mullerian Hormone (AMH) is one such hormone that plays a significant role in assessing a woman's ovarian reserve and fertility potential. In this comprehensive guide, we will delve into the intricacies of AMH and its impact on fertility, providing you with valuable insights to empower your reproductive health journey.
What is AMH?
Anti-Mullerian Hormone, also known as AMH, is a protein produced by the granulosa cells in the ovarian follicles. It plays a vital role in the development of female reproductive organs during fetal life. In adult women, AMH levels are indicative of the quantity of eggs remaining in the ovaries, known as ovarian reserve.
The Significance of AMH in Fertility Assessment
AMH levels are commonly used as a marker for ovarian reserve, providing valuable information about a woman's reproductive potential. Low AMH levels may indicate a reduced ovarian reserve, which can affect fertility and the chances of successful conception. Understanding your AMH levels can help in planning for future fertility treatments and making informed decisions about family planning.
How AMH Impacts Reproductive Health
The impact of AMH on reproductive health extends beyond fertility assessment. Research suggests that AMH levels may also be linked to various reproductive health conditions, such as polycystic ovary syndrome (PCOS) and endometriosis. Monitoring AMH levels can aid in the early detection and management of these conditions, promoting better reproductive outcomes.
Key Insights for Your Reproductive Health
1. Consult with a Fertility Specialist: If you are planning to start a family or have concerns about your fertility, consulting with a fertility specialist can provide valuable insights into your reproductive health. They can perform tests, including AMH level assessments, to evaluate your fertility potential.
2. Understand Your AMH Levels: Knowing your AMH levels can help you make informed decisions about fertility treatments and family planning. If your AMH levels are low, discussing options with your healthcare provider can guide you towards the most suitable path for achieving your reproductive goals.
3. *ifestyle Factors: Maintaining a healthy lifestyle can positively impact your reproductive health. Factors such as diet, exercise, and stress management play a crucial role in optimizing fertility outcomes. Making healthy choices can support your reproductive journey.
4. Stay Informed: Stay informed about the latest advancements in reproductive medicine and fertility treatments. Knowledge is empowering, and being aware of your options can help you navigate the complexities of fertility treatment with confidence.
Understanding AMH and its impact on fertility is essential for anyone looking to take control of their reproductive health. By familiarizing yourself with the role of AMH, seeking professional guidance, and making informed decisions, you can embark on a journey towards achieving your reproductive goals with confidence and clarity.
Remember, your reproductive health is a vital aspect of your overall well-being. By prioritizing education, awareness, and proactive care, you can empower yourself to make informed choices that support your fertility and overall health.
Navigating Relationship Changes After Baby: Tips for Couples Adjusting to Parenthood

Welcoming a new baby into the family is a joyous and transformative experience, but it also brings significant changes to the dynamics of a relationship. The transition to parenthood can be both rewarding and challenging for couples as they navigate the responsibilities, emotions, and adjustments that come with caring for a newborn. In this article, we will explore valuable tips and insights to help couples effectively navigate relationship changes after having a baby and strengthen their bond as they adjust to parenthood.
Understanding Relationship Changes After Baby
The arrival of a baby can bring about a range of changes in a couple’s relationship dynamics. Some common shifts that couples may experience include:
1. Increased Stress: The demands of caring for a newborn, lack of sleep, and adjustments to new routines can lead to heightened stress levels for both partners.
2. Shift in Priorities: With the focus now on the baby’s needs, couples may find themselves reevaluating their individual and shared priorities.
3. Communication Challenges: Effective communication may become more challenging as couples navigate new responsibilities and emotions.
4. Physical and Emotional Exhaustion: The physical and emotional demands of caring for a newborn can take a toll on both partners, impacting their energy levels and emotional well-being.
Tips for Couples Adjusting to Parenthood
1. Prioritize Communication: Make time to openly communicate with your partner about your feelings, concerns, and needs. Effective communication is key to understanding each other’s perspectives and working together as a team.
2. Share Responsibilities: Divide caregiving responsibilities and household tasks equitably to prevent one partner from feeling overwhelmed. Collaborating and supporting each other in childcare duties can strengthen your bond.
3. Take Time for Self-Care: Prioritize self-care to maintain your physical and emotional well-being. Carve out moments for relaxation, hobbies, and personal time to recharge and prevent burnout.
4. Plan Quality Time Together: Despite the demands of parenthood, make an effort to spend quality time as a couple. Schedule date nights, engage in activities you both enjoy, and nurture your relationship outside of parenting responsibilities.
5. Seek Support: Don’t hesitate to seek support from family, friends, or professional resources if you’re feeling overwhelmed. Joining parenting groups or seeking counseling can provide valuable insights and guidance.
6. Celebrate Milestones: Acknowledge and celebrate the small victories and milestones in your relationship and parenthood journey. Express gratitude and appreciation for each other’s efforts and contributions.
7. Stay Patient and Flexible: Remember that adjusting to parenthood is a process, and it’s normal to experience challenges along the way. Stay patient with yourself and your partner, and be willing to adapt and learn together.
Strengthening Your Relationship After Baby
While the post-baby period can present its share of challenges, it also offers couples an opportunity to deepen their connection, grow together, and nurture a strong and resilient relationship. By approaching the changes with understanding, patience, and open communication, couples can navigate the transition to parenthood with grace and unity.
Navigating relationship changes after having a baby requires effort, empathy, and mutual support from both partners. By prioritizing communication, sharing responsibilities, practicing self-care, and celebrating moments of connection, couples can successfully adjust to parenthood and cultivate a loving and harmonious relationship.
Remember, the journey of parenthood is a shared adventure that can strengthen the bond between partners and create lasting memories of love and growth.
“Exploring the Connection Between Menopause and Breast Cancer: Myths, Facts, and Awareness”

Menopause and Breast Cancer: Is There a Link?
Menopause is a natural phase in a woman’s life that signals the end of her reproductive years. During this transition, hormonal changes occur, impacting various aspects of a woman’s health. One common concern among women approaching or experiencing menopause is the potential link between menopause and breast cancer. In this article, we will explore the connection between menopause and breast cancer, separating myths from facts and raising awareness about this important topic.
Understanding Menopause and Breast Cancer
Menopause typically occurs in women between the ages of 45 and 55, marking the cessation of menstruation and a decline in hormone levels, particularly estrogen and progesterone. Breast cancer, on the other hand, is the abnormal growth of cells in the breast tissue, which can lead to the formation of tumors. Research suggests that there may be a relationship between menopause and an increased risk of breast cancer, although the exact mechanisms are still being studied.
Factors Influencing the Link Between Menopause and Breast Cancer
Several factors can influence the potential link between menopause and breast cancer risk. These factors include:
1. Hormonal Changes: The decrease in estrogen levels during menopause may impact breast tissue and contribute to the development of breast cancer.
2. Age: The risk of breast cancer increases with age, and menopausal women are more likely to develop the disease.
3. Family History: A family history of breast cancer can also play a role in an individual’s risk, regardless of menopausal status.
4. Lifestyle Factors: Factors such as diet, exercise, alcohol consumption, and smoking can affect breast cancer risk during menopause.
Myth vs. Fact: Debunking Common Misconceptions
Myth: Menopause Causes Breast Cancer
Fact: Menopause itself does not cause breast cancer. However, the hormonal changes associated with menopause may influence the development of breast cancer in some women.
Myth: All Menopausal Women Will Develop Breast Cancer
Fact: While menopause may be a risk factor for breast cancer, not all menopausal women will develop the disease. Regular screenings and early detection are crucial for effective management.
Myth: Hormone Replacement Therapy (HRT) Always Increases Breast Cancer Risk
Fact: The use of hormone replacement therapy (HRT) during menopause may slightly increase the risk of breast cancer. It is important to discuss the potential risks and benefits of HRT with a healthcare provider.
Importance of Awareness and Early Detection
Raising awareness about the link between menopause and breast cancer is essential for women’s health. Regular breast screenings, such as mammograms and self-exams, can aid in the early detection of breast cancer, improving treatment outcomes and survival rates. Healthcare providers play a crucial role in educating menopausal women about breast health and the importance of proactive screenings.
While the relationship between menopause and breast cancer is complex, being informed and proactive about breast health is key for women navigating this life stage. By understanding the risk factors, debunking myths, and prioritizing regular screenings, menopausal women can take control of their breast health and well-being. Together, we can promote awareness, early detection, and support for women facing the intersection of menopause and breast cancer.
Remember, knowledge is power when it comes to protecting your breast health during menopause.
Newborns in Your 40s: Challenges, Joys, and Considerations for Older Parents

Bringing a newborn into the world is a life-changing experience, filled with both challenges and joys. For parents in their 40s, embarking on the journey of parenthood later in life comes with unique considerations and opportunities. In this article, we will explore the challenges, joys, and important considerations for older parents welcoming newborns in their 40s.
The Decision to Have a Baby in Your 40s
Deciding to have a baby in your 40s is a significant choice that many individuals and couples face. While there may be challenges associated with later parenthood, such as decreased fertility and increased health risks, there are also numerous joys and benefits that come with raising a child at this stage of life.
Challenges Faced by Older Parents
1. Fertility Concerns: As individuals age, fertility declines, making it more challenging to conceive naturally. Assisted reproductive technologies, such as IVF, may be necessary for older parents.
2. Health Risks: Older parents may face higher risks of pregnancy complications, such as gestational diabetes, hypertension, and chromosomal abnormalities in the baby.
3. Energy Levels: Parenting a newborn requires significant energy and stamina, which may be more challenging for older parents.
4. Long-Term Planning: Older parents may need to consider their own health and longevity when planning for their child's future.
Joys of Parenting in Your 40s
1. Emotional Maturity: Older parents often bring a wealth of life experience and emotional maturity to their parenting journey.
2. Financial Stability: Parents in their 40s may be more financially secure and able to provide for their child's needs.
3. Quality Time: Older parents may have established careers and be able to prioritize quality time with their child.
4. Life Perspective: Parenting later in life can bring a unique perspective and appreciation for the joys of raising a child.
Considerations for Older Parents
1. Health and Wellness: Prioritize your health and well-being to ensure you have the energy and vitality to care for your newborn.
2. Support System: Build a strong support network of family and friends to help you navigate the challenges of parenthood.
3. Financial Planning: Consider the long-term financial implications of raising a child and plan accordingly.
4. Open Communication: Have open and honest conversations with your partner and healthcare provider about your decision to have a baby in your 40s.
Embracing the Journey of Parenthood
Welcoming a newborn into your life in your 40s is a unique and rewarding experience that comes with its own set of challenges and joys. By acknowledging the considerations, seeking support, and embracing the journey with an open heart, older parents can navigate the path of parenthood with confidence and love.
Parenting a newborn in your 40s is a deeply fulfilling and transformative experience that brings both challenges and joys. By approaching the journey with patience, resilience, and love, older parents can create a nurturing and supportive environment for their child to thrive and grow.
Remember, age is just a number when it comes to the boundless love and joy that parenthood brings.
