Month: October 2023
Pre-Labor Symptoms: Understanding Flu-Like Signs Before Labor
As your due date approaches, you may start experiencing a range of physical discomforts and changes. It is not uncommon for expectant mothers to experience flu-like symptoms shortly before going into labor. While it can be challenging to distinguish between normal pregnancy discomforts and pre-labor signs, understanding these flu-like symptoms can help you prepare for the imminent arrival of your little one. In this comprehensive guide, we will explore the various flu-like signs that may occur before labor and provide insights into their significance.
Recognizing Flu-Like Symptoms Before Labor:
- Increased Fatigue: Feeling exceptionally tired or experiencing a sudden surge of exhaustion can be a sign that labor is approaching. This fatigue may be more intense than the usual pregnancy-related tiredness.
- Body Aches and Joint Pain: Similar to the flu, some women may experience body aches and joint pain before labor. These discomforts may be more noticeable in the lower back, pelvis, or hips.
- Gastrointestinal Disturbances: Pre-labor can bring about digestive changes such as nausea, vomiting, diarrhea, or an upset stomach. These symptoms are often attributed to hormonal fluctuations and the body’s preparation for childbirth.
- Flu-like Chills and Fever: It is not uncommon for pregnant women to experience flu-like chills and a low-grade fever before labor. These symptoms can be a result of hormonal changes and the body’s natural response to impending childbirth.
Causes and Explanations:
- Hormonal Shifts: As labor approaches, the body undergoes hormonal changes that can mimic flu-like symptoms. The release of prostaglandins and other hormones prepares the body for labor, causing various physical reactions.
- Increased Immune System Activity: The immune system becomes more active in the final stages of pregnancy, which can lead to flu-like symptoms. This heightened immune response is a natural protective mechanism to support the upcoming labor and delivery.
- Progesterone Withdrawal: The decrease in progesterone levels as labor nears can contribute to flu-like symptoms. Progesterone, a hormone essential for maintaining pregnancy, decreases as the body prepares for childbirth.
Differentiating Pre-Labor Symptoms from Illness:
It is crucial to differentiate between pre-labor symptoms and an actual illness. While flu-like signs before labor may resemble common illnesses, there are some key distinctions to consider:
- Duration and Intensity: Pre-labor symptoms are usually temporary and may come and go. They are often more intense than typical pregnancy discomforts but tend to subside as labor progresses.
- Absence of Other Illness Symptoms: Unlike the flu or other illnesses, pre-labor symptoms are usually not accompanied by respiratory symptoms like coughing or sneezing. If you experience respiratory symptoms, it is important to consult your healthcare provider.
- Progression of Symptoms: Pre-labor symptoms may intensify and become more frequent over time, indicating that your body is preparing for labor. If you notice a significant change in symptoms or are unsure, it is advisable to seek medical advice.
Coping Strategies and Self-Care:
While pre-labor symptoms can be uncomfortable, there are several self-care strategies that can help alleviate discomfort and prepare your body for labor:
- Rest and Relaxation: Prioritize rest and relaxation to combat fatigue and promote overall well-being.
- Take frequent breaks, engage in calming activities, and ensure you are getting enough sleep.
- Warm Baths or Showers: A warm bath or shower can help ease body aches and provide temporary relief from flu-like symptoms. However, avoid hot water that could raise your body temperature excessively.
- Hydration and Nutrition: Stay hydrated by drinking plenty of water and consuming a balanced diet. Opt for light, easily digestible meals and incorporate foods rich in essential nutrients to support your body during this stage.
- Gentle Exercise: Engaging in gentle exercises, such as walking or prenatal yoga, can help alleviate discomfort and improve circulation. Consult your healthcare provider for specific exercise recommendations.
When to Seek Medical Attention:
While pre-labor symptoms are usually a normal part of the birthing process, it is essential to be aware of warning signs that may require medical attention:
- Severe or Prolonged Symptoms: If your symptoms are severe, persistent, or worsen over time, it is important to consult your healthcare provider. This can help rule out any underlying health concerns.
- Signs of Illness: If you experience symptoms commonly associated with illnesses, such as a high fever, severe respiratory symptoms, or vomiting, it is crucial to seek immediate medical attention.
- Bleeding or Leakage of Fluid: If you notice any vaginal bleeding or a sudden gush or trickle of fluid, it could indicate a rupture of the amniotic sac. Contact your healthcare provider or go to the hospital as soon as possible.
Experiencing flu-like symptoms before labor is a common occurrence for many expectant mothers. Understanding the causes, differentiating these symptoms from illnesses, and adopting self-care strategies can help you navigate this stage of your pregnancy with confidence and peace of mind. Remember to consult your healthcare provider if you have any concerns or experience severe symptoms. Soon, you will be welcoming your little one into the world, and these pre-labor discomforts will be a distant memory.
Optimal Postpartum Diet for New Moms: Essential Tips and Guidelines

Welcoming a new baby into the world is an incredible experience, but it can also take a toll on a mother’s body. After giving birth, it is essential for new moms to focus on their physical and mental well-being. One crucial aspect of this recovery process is maintaining a healthy diet that supports postpartum healing and provides the necessary nutrients for both mom and baby. In this article, we will discuss the optimal postpartum diet for new moms and provide essential tips and guidelines to help them navigate this transformative period.
1. Prioritize Nutrient-Dense Foods
A nutrient-dense diet is crucial during the postpartum period as it helps replenish the body’s stores, support healing, and promote milk production. Include a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats in your meals. Focus on foods that are rich in essential vitamins and minerals such as iron, calcium, vitamin D, and omega-3 fatty acids. Leafy greens, nuts, seeds, legumes, and fish like salmon are excellent sources of these nutrients.
2. Stay Hydrated
Staying hydrated is vital for new moms, especially if they are breastfeeding. Breast milk production requires an adequate intake of fluids. Aim to drink at least eight to ten glasses of water or other hydrating beverages like herbal teas throughout the day. Avoid sugary drinks and caffeinated beverages as they can dehydrate your body.
3. Include Protein-Rich Foods in Postpartum Diet
Protein plays a crucial role in postpartum recovery and breastfeeding. It helps repair tissues, boost energy levels, and support the growth and development of the baby. Incorporate lean sources of protein such as chicken, turkey, fish, eggs, tofu, and legumes into your meals. Greek yogurt and cottage cheese are also excellent options that provide protein and calcium.
4. Don’t Skip Healthy Fats
Healthy fats are an essential part of a postpartum diet as they provide energy and support brain development in the baby. Include foods like avocados, nuts, seeds, olive oil, and fatty fish in your meals. These healthy fats also help in the absorption of fat-soluble vitamins like vitamin D, which is crucial for bone health.
5. Eat Small, Frequent Meals
New moms often find it challenging to sit down for a full meal due to the demands of their newborn. Eating small, frequent meals throughout the day can help ensure a steady supply of nutrients and energy. Prepare healthy snacks and keep them readily available, like cut-up fruits, nuts, yogurt, or whole grain crackers. This approach will also help stabilize blood sugar levels and prevent energy crashes.
6. Limit Processed Foods and Added Sugars
Processed foods and added sugars offer little to no nutritional value and can hinder postpartum recovery. These foods can lead to weight gain, low energy levels, and may even impact your mood. Instead, opt for whole, unprocessed foods that provide essential nutrients without unnecessary additives. Choose natural sweeteners like honey or maple syrup instead of refined sugar when sweetening foods or beverages.
7. Focus on Fiber-Rich Foods
A postpartum diet should include an adequate amount of dietary fiber to prevent constipation, a common issue among new moms. Fiber-rich foods like whole grains, fruits, vegetables, and legumes help regulate bowel movements and promote a healthy digestive system. Additionally, they contribute to feelings of fullness and aid in weight management.
8. Consider Nutritional Supplements in Postpartum Diet
While a well-balanced diet should ideally provide all the necessary nutrients, some new moms may need additional support. Consult with your healthcare provider to determine if you require any specific supplements, such as iron or vitamin D, to address any deficiencies. It is crucial to avoid self-prescribing supplements as excessive amounts can be harmful.
9. Practice Mindful Eating
Amidst the chaos of caring for a newborn, it is essential to practice mindful eating. Slow down and savor each bite, paying attention to your body’s hunger and fullness cues. This practice can help prevent overeating, aid digestion, and allow you to enjoy your meals more fully. Eating in a calm and relaxed environment can also contribute to better digestion.
10. Get Adequate Rest and Support
While not directly related to diet, rest and support are crucial for postpartum recovery. Lack of sleep can lead to poor food choices and hinder the body’s healing process. Enlist the help of family and friends to assist with household chores and caring for the baby. Take naps whenever possible and prioritize self-care to ensure you have the energy to maintain a healthy diet and care for your little one.
The postpartum period is a time of immense change and adjustment for new moms. Prioritizing a nutrient-dense diet, staying hydrated, and eating small, frequent meals can aid in postpartum recovery, boost energy levels, and support breastfeeding. Additionally, avoiding processed foods, practicing mindful eating, and seeking adequate rest and support are essential for overall well-being. Remember, every woman’s postpartum journey is unique, so consult with your healthcare provider to tailor a diet plan that suits your specific needs and helps you thrive during this transformative time.
“Postpartum Ovulation: Recognizing the Signs of Ovulation After Giving Birth”
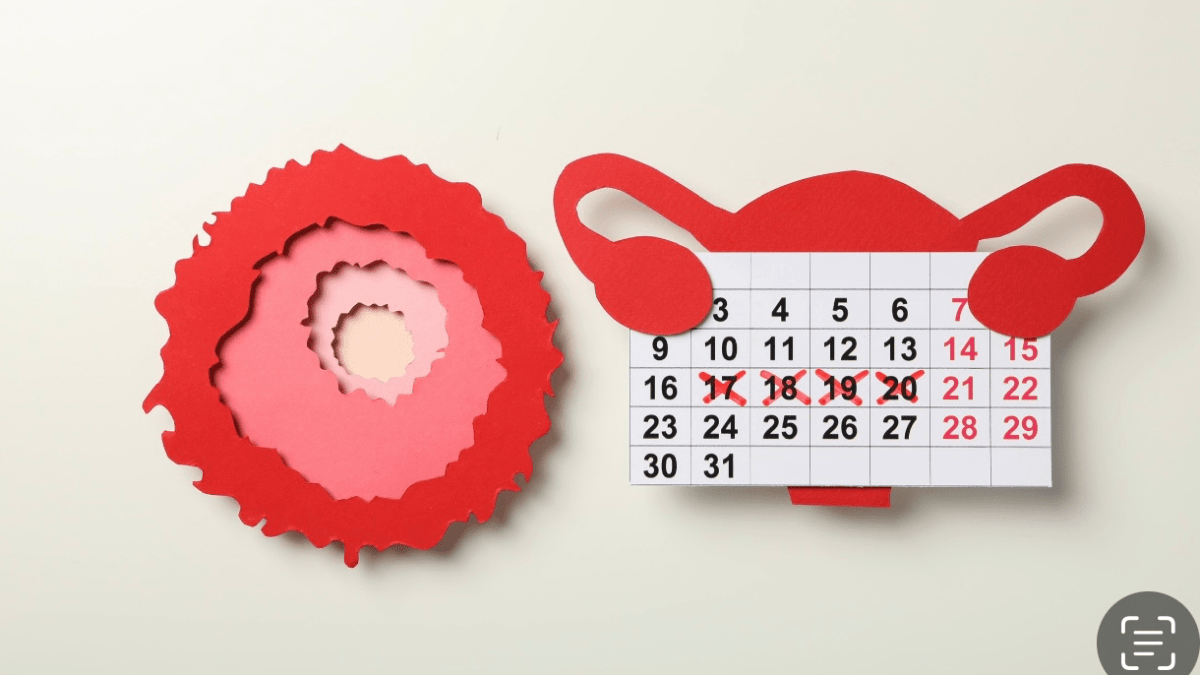
After giving birth, many women wonder when their menstrual cycle will resume and when they will ovulate again. Understanding the signs of ovulation during the postpartum period is essential for those planning to conceive or simply monitoring their fertility. In this comprehensive article, we will explore the topic of postpartum ovulation, its timing, and the various signs and symptoms to look out for. By recognizing these signs, women can gain valuable insights into their fertility and make informed decisions about family planning.
1. The Timing of Ovulation After Giving Birth
Ovulation usually resumes at different times for women who have given birth. For some, it may occur within a few weeks after delivery, while others may experience a longer delay. The return of ovulation depends on various factors, including whether or not the woman is breastfeeding. Exclusive breastfeeding can suppress ovulation and delay the return of menstrual cycles, while formula feeding or introducing solid foods may lead to earlier ovulation. It is important to note that even if ovulation has not occurred, it is still possible to conceive, as the first ovulation after giving birth can happen before the first menstrual period.
2. Signs and Symptoms of Ovulation
Recognizing the signs and symptoms of ovulation can help women identify their fertile window. Some common signs include:
a. Changes in cervical mucus: As ovulation approaches, the cervical mucus becomes clearer, stretchier, and similar to raw egg whites. This is known as “fertile” cervical mucus and indicates increased fertility.
b. Increased basal body temperature (BBT): Tracking your BBT can reveal a slight rise in temperature after ovulation. This rise is caused by an increase in progesterone levels and can be detected using a basal body thermometer.
c. Ovulation pain or Mittelschmerz: Some women experience mild pelvic pain or twinges on one side of their lower abdomen during ovulation. This sensation, known as Mittelschmerz, can help indicate the release of an egg.
d. Changes in libido: Many women notice an increase in sexual desire around the time of ovulation. This heightened libido is thought to be nature’s way of encouraging conception.
3. Charting and Tracking Ovulation
Charting and tracking ovulation can provide valuable insights into a woman’s fertility patterns. Several methods can be used:
a. Ovulation predictor kits (OPKs): These kits detect the surge in luteinizing hormone (LH) that occurs just before ovulation. By following the instructions provided, women can identify their most fertile days.
b. Basal body temperature (BBT) charting: Tracking daily temperatures can help pinpoint ovulation. A slight increase in BBT indicates that ovulation has occurred.
c. Cervical mucus observation: Monitoring changes in cervical mucus consistency and appearance can help predict ovulation. Women can record these changes on a fertility chart.
d. Smartphone apps and fertility trackers: Numerous smartphone apps and fertility trackers are available to help women record and analyze their menstrual cycles, basal body temperatures, and other fertility signs.
4. Factors Affecting Postpartum Ovulation
Several factors can influence the return of ovulation after giving birth. Breastfeeding, as mentioned earlier, can delay ovulation due to the production of the hormone prolactin. Stress, hormonal imbalances, and individual variations in reproductive systems can also impact the timing of ovulation. It is important to remember that even if ovulation has not resumed, contraception should still be considered if pregnancy is not desired.
Recognizing the signs of ovulation after giving birth is crucial for women who are planning to conceive or simply tracking their fertility. Understanding the timing of ovulation, as well as the signs and symptoms to look out for, can empower women to make informed decisions about family planning. By utilizing tracking methods such as charting basal body temperature, observing changes in cervical mucus, or using ovulation predictor kits, women can gain valuable insights into their fertility patterns. Remember, consulting with a healthcare professional is always recommended for personalized advice and guidance regarding postpartum ovulation.
Endometriosis Self-Care: A Comprehensive Guide to Managing Symptoms and Improving Quality of Life

Living with endometriosis can be challenging, but incorporating effective self-care practices into your daily routine can help manage symptoms and improve your overall quality of life. In this comprehensive guide, we will explore various self-care strategies and techniques that can assist you in coping with endometriosis. From dietary adjustments and exercise routines to stress management and alternative therapies, we will provide valuable insights and practical tips to help you navigate this condition more effectively.
1. Understanding Endometriosis
Before delving into self-care techniques, it is crucial to have a basic understanding of endometriosis. Endometriosis is a chronic condition where tissue similar to the lining of the uterus grows outside the uterus. This can lead to severe pelvic pain, painful periods, fatigue, and fertility issues. While there is no cure for endometriosis, self-care practices can help alleviate symptoms and improve overall well-being.
2. Diet and Nutrition
Adopting a healthy, well-balanced diet is an essential aspect of endometriosis self-care. Certain foods can trigger inflammation and worsen symptoms, while others have anti-inflammatory properties that can provide relief. Incorporate foods rich in omega-3 fatty acids, such as fatty fish, walnuts, and flaxseeds, as they can help reduce inflammation. Avoid or limit foods high in trans fats, processed sugars, and caffeine, as they may exacerbate symptoms. Additionally, staying hydrated and consuming plenty of fiber can aid in regulating hormones and managing gastrointestinal issues commonly associated with endometriosis.
3. Exercise and Movement
Regular physical activity can play a vital role in managing endometriosis symptoms. Engaging in low-impact exercises like walking, swimming, or yoga can help reduce pain and inflammation, improve circulation, and boost mood. It is essential to listen to your body and avoid high-impact activities that may cause discomfort. Incorporating gentle stretching exercises can also help relieve muscle tension and promote relaxation.
4. Stress Management
Stress can aggravate endometriosis symptoms, so implementing stress management techniques is crucial for self-care. Explore relaxation techniques such as deep breathing exercises, meditation, or mindfulness practices to reduce stress levels. Engaging in activities you enjoy, such as reading, painting, or spending time in nature, can also provide a much-needed mental and emotional break. Prioritizing self-care activities and setting boundaries in your daily life can help reduce stress and improve overall well-being.
5. Alternative Therapies for Endometriosis Self-Care
Many individuals with endometriosis find relief through various alternative therapies. Acupuncture, for example, has been shown to help alleviate pain and regulate menstrual cycles. Herbal remedies, such as chamomile tea or turmeric supplements, may also provide anti-inflammatory benefits. Consult with a qualified healthcare professional before trying any alternative therapies to ensure they are safe and suitable for your specific condition.
Incorporating effective self-care practices into your routine can significantly enhance your ability to manage endometriosis symptoms and improve your overall quality of life. If ignored, endometriosis can lead to ectopic pregnancy. From making dietary adjustments and engaging in regular exercise to implementing stress management techniques and exploring alternative therapies, there are various approaches to consider. Remember, self-care is a personal journey, and it may take time to find the strategies that work best for you. By prioritizing your well-being and seeking support from healthcare professionals, you can navigate the challenges of endometriosis with greater resilience and positivity.
How Long Does hCG Rise After Implantation?

Understanding the timing of hCG (human chorionic gonadotropin) rise after implantation is crucial for women who are trying to conceive or suspect they may be pregnant. hCG is a hormone produced by the placenta after implantation occurs, and its levels can be detected through pregnancy tests. In this comprehensive guide, we will delve into the process of hCG rise after implantation, providing insights into the timing, factors influencing hCG levels, and the significance of hCG in pregnancy.
I. The Process of Implantation and hCG Production
A. Implantation:
1. After fertilization, the fertilized egg travels down the fallopian tube and into the uterus.
2. Implantation occurs when the fertilized egg attaches to the uterine lining.
3. Following successful implantation, the placenta begins to develop, which is responsible for hCG production.
B. hCG Production:
1. The trophoblast cells of the developing placenta produce hCG.
2. hCG serves to support the production of progesterone, which is vital for maintaining the pregnancy.
3. hCG levels increase rapidly during the early stages of pregnancy.
II. Timing of hCG Rise After Implantation
A. Early hCG Levels:
1. After implantation, hCG levels are generally too low to be detected by pregnancy tests.
2. It takes some time for hCG levels to increase enough to be detectable.
B. When to Take a Pregnancy Test:
1. Most pregnancy tests can detect hCG levels around 10-14 days after conception.
2. However, the accuracy of the test may vary, and it is best to follow the instructions provided by the test manufacturer.
C. hCG Levels Over Time:
1. hCG levels double every 48-72 hours during the early stages of pregnancy.
2. The rate of hCG rise varies from woman to woman but generally follows a consistent pattern.
III. Factors Influencing hCG Levels
A. Gestational Age:
1. hCG levels tend to be higher in later stages of pregnancy.
2. Early in pregnancy, hCG levels increase rapidly, but the rate slows down as the pregnancy progresses.
B. Multiple Pregnancies:
1. Women carrying multiples, such as twins or triplets, tend to have higher hCG levels compared to those carrying a single fetus.
2. The presence of multiple embryos stimulates increased hCG production.
C. Ectopic Pregnancy:
1. In ectopic pregnancies, where the fertilized egg implants outside the uterus, hCG levels may rise more slowly or be lower than expected.
2. Monitoring hCG levels in cases of suspected ectopic pregnancy is crucial for early detection and appropriate medical intervention.
IV. The Significance of hCG in Pregnancy
A. Confirmation of Pregnancy:
1. hCG is a reliable marker for confirming pregnancy, especially when detected through a pregnancy test.
2. Rising hCG levels indicate a viable pregnancy.
B. Monitoring Pregnancy Progression:
1. Serial hCG measurements can provide insights into the progression of a pregnancy.
2. Slower than expected hCG rise or a decline in hCG levels may indicate potential complications.
C. Assessing Pregnancy Viability:
1. hCG levels should increase steadily during early pregnancy.
2. A lack of hCG rise or a significant decrease may suggest a non-viable pregnancy, such as a miscarriage.
Understanding the timeline of hCG rise after implantation is essential for women trying to conceive or those who suspect they may be pregnant. While hCG levels can vary among individuals, the general pattern of doubling every 48-72 hours provides a useful guideline. By monitoring hCG levels and seeking medical advice if any concerns arise, women can ensure the best possible care for themselves and their growing pregnancy.
Understanding PCOS and Ectopic Pregnancy: Causes, Symptoms and Treatments

It takes a lot of commitment & effort for a human to remain healthy. However, it is not a simple task for a female. There are two primary reasons why men’s and women’s body types differ significantly. Ectopic pregnancy and polycystic ovarian syndrome (PCOS) are the two conditions that women face. These are the two prevalent disorders of the reproductive system that have an impact on the general health of the female body’s organs. PCOS is a hormonal condition characterized by tiny cysts and enlarged ovaries. On the contrary, ectopic pregnancy happens when an egg that has been fertilized implants outside of the uterus. So read this extensive guide to gain a thorough understanding of PCOS and ectopic pregnancy treatment, as well as the conditions’ underlying causes, effects on women’s health, and management options.
What is PCOS?
Today, PCOS, or polycystic ovarian syndrome, is one of the most common medical conditions affecting women. Nowadays, women usually lead extremely hectic lifestyles that are stressful and full of various activities. PCOS is identified when a person neglects their mental, physical, and organ health. (PCOS) is a medical condition where the ovaries generate male sex hormones, or androgens, excessively. Women normally produce small amounts of these hormones. In addition, high levels of testosterone and insulin lead to a hormonal imbalance in the bodies of women.
What is the cause of PCOS?
The exact root cause of PCOS is yet unknown. Although there isn’t a single cause for PCOS, numerous studies, examinations, and medical expert’s advice have identified a few possible causes.
- The female body’s resistance to insulin
- Higher levels of androgen
- PCOS tends to run in families which means it can be an inherited trait.
- Obesity and constant junk food consumption
Symptoms of PCOS
- The irregular menstrual cycle is one of the initial signs of PCOS patients. Women with PCOS, according to doctors, miss their periods for weeks at a time and, in certain cases, for months.
- The female body has an overabundance of hair growth. Particularly on the face, neck, stomach, and other body areas, hair grows & thickens.
- Acne and oily skin are other symptoms of PCOS. Skin gets dull because of hormone imbalances and irregular periods.
- Beyond all other symptoms, females with PCOS have trouble losing weight since they gain it quickly and find it difficult to lose.
What are the best Treatment Options available for PCOS?
- Making lifestyle adjustments is the first and best course of action, and it can only be taken by the patient independently. Therefore, women with PCOS must improve their lifestyles by including a healthy diet, regular exercise, weight control techniques, getting enough sleep, and reducing stress.
- See an experienced gynecologist and follow their recommendations. Medications are also included based on the severity of your PCOS.
- Women with PCOS who are unable to conceive should speak with reliable medical professionals and begin their reproductive treatments as directed.
What is Ectopic Pregnancy?
When a fertilized egg implants itself outside of the womb, usually in one of the fallopian tubes, the condition is known as ectopic pregnancy. This circumstance differs from a typical pregnancy. Fallopian tubes are tubes that connect the ovaries to the womb. If an egg gets stuck in it, that won’t develop into a baby and could endanger the mother’s health if the pregnancy continues.
Causes of Ectopic Pregnancy
- The fallopian tube is damaged.
- scarring or blockage in the fallopian tube
- Hormone abnormalities that impact the fertilization of the egg
- Increased dangers for females who have had one ectopic pregnancy
What are the Symptoms of Ectopic Pregnancy?
- The most common symptom of an ectopic pregnancy is vaginal bleeding, which can range from light to heavy and is typically accompanied by pelvic pain.
- Due to internal bleeding shoulder pain also occurs often as the fallopian tube ruptures.
- Sharp or one-sided lower abdominal pain is another typical symptom that most women with the condition experience.
- Another sign of the illness is discomfort when urinating or defecating.
What are the best Treatment Options available for Ectopic Pregnancy?
- It’s crucial to speak with an experienced gynecologist and then start with taking medications as prescribed by your doctor.
- Laparoscopic surgery is often necessary when a woman’s health is at risk.
- In certain cases, doctors may recommend future pregnancies based on the harm caused by the first ectopic pregnancy.
Relationship Between PCOS and Ectopic Pregnancy
There is a correlation between the two conditions, and a female who has one may be more susceptible to developing the other.
- Ectopic pregnancies are more likely in women with PCOS.
- Hormonal imbalances that contribute to PCOS can also affect the fertilized egg’s journey through the fallopian tubes.
- PCOS should never be viewed as an uncomplicated condition that can be cured easily—because, it may cause problems with pregnancy. It may raise the chance of scarring and blockage of the fallopian tube, which may lead to an ectopic pregnancy.
How PCOS Can be Managed to Reduce Ectopic Pregnancy Risk?
Every medical condition has a treatment of some sort, and PCOS and ectopic pregnancy are no exception. The following are some pointers for managing PCOS to lower the chance of an ectopic pregnancy:
- Women must have routine monitoring. Ultrasounds, testing, and important routine examinations should be undertaken to detect any possible issues.
- Seek immediate medical attention from your physician if you experience any symptoms that may indicate PCOS.
- To reduce the risk of problems including ectopic pregnancy, prioritize early treatment of PCOS.
- Make lifestyle adjustments, get the proper medical attention, exercise, eat a nutritious diet, and follow your doctor’s recommendations.
Thus, we know that complicated reproductive health issues like PCOS and ectopic pregnancy can have a big influence on a woman’s life. However, for efficient management and prevention of complications, it is essential to understand their causes, symptoms, and available treatments. Through proactive measures such as changes in lifestyle, medication, and fertility treatments, women can address PCOS and improve their reproductive health and overall well-being. Ectopic pregnancies can also be quickly identified and treated. The majority of aspects concerning PCOS and ectopic pregnancy have been covered in this guide, but you can check out our other comprehensive articles. Check our other blogs to get all the specifics.
Pregnancy Yoga: An essential Guide for Expecting Mothers

You’re expecting?! Congratulations! You must be – excited, scared, happy, and overwhelmed – all at the same time. It’s difficult to put your finger on just what you’re feeling, isn’t it? The kicks are delightful, but the cramps are debilitating. You might be glowing with enthusiasm one moment and overcome with emotion the next. Nothing quite explains the feeling of having a life growing inside you. You may also experience a fair share of mood swings; courtesy of hormonal changes. This is precisely why yoga can be a godsend for you during pregnancy.
How Yoga for Pregnant Women Helps
- Yoga provides holistic health benefits for soon to-be-mothers:
- Yoga during pregnancy helps keep the body supple. They relieve tension around the cervix by opening up the pelvic region. This prepares to-be mothers for labor and delivery.
- Yoga and pranayamas can train you to breathe deeply and relax consciously, helping you face the demands of labor and childbirth.
- Pregnancy Yoga helps alleviate the effect of common symptoms such as morning sickness, painful leg cramps, swollen ankles, and constipation.
Yoga asanas also help pregnant women recover faster post-delivery Pregnancy is a beautiful journey that brings numerous physical and emotional changes for women. As an expecting mother, it’s important to prioritize your health and well-being during this crucial time. One highly recommended activity is practicing yoga, which not only helps you stay physically fit but also provides mental and emotional benefits. In this comprehensive guide, we will delve into the world of pregnancy yoga and explore its various aspects, benefits, and safety precautions.
Understanding Pregnancy Yoga:
Pregnancy yoga, also known as prenatal yoga, is a specialized form of yoga tailored to the needs and limitations of expectant mothers. It involves gentle stretching, breathing exercises, and relaxation techniques that promote physical strength, flexibility, and emotional balance. Pregnancy yoga classes are typically designed to address the specific physical changes and challenges that occur during each trimester.
Physical Benefits:
Regular practice of pregnancy yoga offers numerous physical benefits. It helps alleviate common discomforts such as back pain, fatigue, and swollen ankles. The gentle stretches and poses improve blood circulation, reduce muscle tension, and promote overall strength and flexibility. Additionally, it can enhance posture and help prepare the body for childbirth.
Emotional and Mental Benefits:
Pregnancy can be an emotional rollercoaster, and yoga provides a safe space for expectant mothers to connect with their bodies and emotions. The breathing techniques and meditation practiced in pregnancy yoga help reduce stress, anxiety, and mood swings. It promotes relaxation, inner peace, and a sense of well-being, which can be incredibly beneficial during pregnancy.
Choosing the Right Pregnancy Yoga Class:
When considering pregnancy yoga, it is essential to find a qualified and experienced instructor who specializes in prenatal yoga. Look for classes that focus on gentle movements, modifications for different stages of pregnancy, and proper breathing techniques. Joining a supportive community of expectant mothers can also provide a nurturing environment for sharing experiences and building friendships.
Safe and Recommended Yoga Poses for Pregnancy:
During pregnancy, certain yoga poses are not suitable or safe. However, many poses can be adapted or modified to accommodate the changing body. Some recommended poses for pregnant women include:
- Cat-Cow Stretch: This gentle spinal movement helps relieve back pain and promotes flexibility.
- Butterfly Pose: Sitting with the soles of your feet together and gently pressing the knees down can help open the hips and relieve tension.
- Prenatal Sun Salutations: Modified versions of the traditional sun salutation sequence help improve circulation, stretch the entire body, and build strength.
- Supported Squat: This pose helps open the pelvis, prepare for childbirth, and strengthen the legs.
It is crucial to listen to your body and only practice poses that feel comfortable. If any pose causes discomfort or pain, it is best to avoid it and consult with your instructor or healthcare provider.
Safety Precautions and Considerations:
- While pregnancy yoga is generally safe, it is essential to take necessary precautions to ensure the well-being of both you and your baby:
- Consult Your Healthcare Provider: Before starting any exercise regimen during pregnancy, it is crucial to seek guidance from your healthcare provider. They can assess your individual situation and provide specific recommendations.
- Avoid Overexertion: Pregnancy is not the time to push your limits. Listen to your body and take breaks when needed. Avoid overheating and stay hydrated during your practice.
- Modify Poses as Needed: As your pregnancy progresses, you may need to modify or avoid certain poses that put pressure on your abdomen or strain your muscles. Always prioritize comfort and safety.
- Avoid Deep Twists and Inversions: Deep twists and inversions should be avoided during pregnancy as they may affect the blood flow to the uterus and potentially harm the baby.
Pregnancy yoga offers expectant mothers a multitude of benefits, both physically and emotionally. It provides a safe and effective way to stay active, relieve discomfort, reduce stress, and connect with the changes happening within your body. By choosing the right class, practicing recommended poses, and following safety precautions, you can enjoy a fulfilling and nourishing experience. Embrace this transformative time and embark on a journey of self-care and well-being through pregnancy yoga.
Newborn Care: Essential Tips and Expert Advice for Caring for Your Baby

Learn how to care for your newborn with these essential tips and expert advice. From feeding and diapering to sleep routines and soothing techniques, this comprehensive guide will help you navigate the beautiful journey of caring for your baby.
Caring for a newborn can be both thrilling and overwhelming. As a parent, you want to ensure your baby receives the best care possible. From feeding and diapering to sleep routines and soothing techniques, understanding the essentials of newborn care is crucial. In this article, we will provide you with expert tips and essential advice to help you navigate the beautiful journey of caring for your newborn.
1. Establish a Feeding Routine:
– Breastfeeding: If you choose to breastfeed, seek guidance from a lactation consultant to ensure proper latching and positioning.
– Formula feeding: Ensure the bottles and nipples are clean, and follow the instructions for preparing formula accurately.
2. Diapering and Hygiene:
– Change diapers frequently to keep your baby clean and comfortable.
– Use gentle baby wipes and diaper rash creams to prevent irritation.
– Establish a bathing routine, using mild and baby-friendly products.
3. Creating a Soothing Environment:
– Swaddling: Wrap your baby snugly in a soft blanket to mimic the womb’s comforting feeling.
– White noise: Use a white noise machine or play soft music to help soothe your baby to sleep.
– Gentle touch and rocking: Physical affection and gentle motion can be calming for newborns.
4. Sleep Routine and Safety:
– Newborns sleep a lot, but establishing a sleep routine can help them differentiate between day and night.
– Ensure your baby’s sleep environment is safe, with a firm mattress, fitted sheet, and no blankets or pillows that pose suffocation hazards.
5. Recognizing and Responding to Cues:
– Newborns communicate through cues like crying, facial expressions, and movements. Learn to recognize their needs and respond promptly.
6. Seeking Professional Support:
– Consult with your pediatrician or healthcare provider for essential check-ups, vaccinations, and any concerns about your baby’s health.
– Join parenting support groups or attend classes to connect with other parents and gain additional knowledge and support.
Caring for your newborn is a beautiful and rewarding journey, but it also comes with many challenges. By following these expert tips and essential advice, you can ensure that your baby receives the best care possible. Remember to trust your instincts as a parent and seek support when needed. With love, patience, and dedication, you will provide a nurturing environment for your baby’s growth and development.
