Month: October 2024
How Soon Can You Dive In? Swimming After a C-Section Explained

Welcoming a baby into the world is an exhilarating experience, but the recovery process, especially after a C-section (cesarean delivery), requires patience, care, and a whole lot of self-love. One common question many new moms have is, “When can I swim after a C-section?” Whether you’re craving a refreshing dip in the pool or simply looking forward to some much-needed relaxation, understanding the best time to dive back in is essential for a smooth recovery.
This guide breaks down everything you need to know about swimming after a C-section, from the healing timeline to safety tips, and why it’s important to let your body fully recover before you take the plunge.
Understanding the Healing Process After a C-Section
Before diving into swimming specifics, it’s important to understand the healing journey following a C-section. A C-section is major abdominal surgery, and while it’s a common procedure, it involves several layers of tissue, muscles, and skin that need time to heal properly.
Here’s a basic breakdown of what happens after your C-section:
– First 1-2 weeks: This is the most critical time for healing. You may experience swelling, bruising, and tenderness around your incision. During this phase, your body is healing from the inside out.
– 2-6 weeks: The surface incision will begin to heal, and you may feel more comfortable moving around. However, the deeper layers of tissue are still recovering.
– 6-8 weeks: Most doctors recommend a postpartum check-up at this time to assess how well your incision has healed. If everything looks good, this is often when you’ll be cleared for light activities.
– Beyond 8 weeks: Full recovery from a C-section can take several months. Even though the incision may look healed on the outside, your body is still working on healing deeper layers of tissue.
When Can You Safely Swim After a C-Section?
The general rule of thumb is that you should wait at least 6-8 weeks after a C-section before going swimming. But before you grab your swimsuit, it’s essential to get the green light from your doctor during your postpartum check-up.
Why 6-8 weeks? During this period:
– Your incision should have healed enough to prevent infection.
– Your body needs time to repair the tissues that were cut during surgery.
– Bleeding (lochia) after childbirth should have completely stopped. Swimming while bleeding increases the risk of infection.
It’s important to remember that every woman’s body heals differently. Some may feel ready sooner, while others may need a bit more time. Always prioritize your own body’s signals and consult your healthcare provider if you’re unsure.
Why Rushing Back to the Pool is Risky
After surgery, your body is in a vulnerable state, and rushing into physical activities like swimming can pose some risks:
1. Infection
The risk of infection is the primary reason for delaying swimming after a C-section. Bodies of water—whether it’s a pool, lake, or ocean—can harbor bacteria. Even if the water is treated with chlorine, it’s not completely sterile, and the risk of introducing bacteria to your healing incision is higher.
2. Incision Irritation
Water can soften the skin around your incision, which may cause irritation or even slow down the healing process. While your scar may seem healed on the outside, the deeper layers are still vulnerable, and prolonged water exposure can disrupt the recovery.
3. Muscle Strain
Swimming is a full-body workout, and although it may feel like a low-impact exercise, it can strain your abdominal muscles, which are still healing from surgery. Engaging your core too soon can lead to discomfort, or worse, injury.
Tips for Swimming After a C-Section
Once you’ve got the go-ahead from your doctor, swimming can be a fantastic way to gently ease back into physical activity. It’s low impact, helps build strength, and can even relieve some of the stress that comes with motherhood. Here are some key tips to keep in mind as you reintroduce swimming to your routine:
1. Start Slow
Even if you feel like diving in and doing laps, take it easy at first. Start with gentle floating or light movements in the water. Allow your body to adjust to being in the water again before increasing intensity.
2. Avoid High-Impact Strokes
Swim strokes like the butterfly or even the breaststroke can put a lot of strain on your core. Start with gentler strokes, like the backstroke or sidestroke, which minimize strain on your abdomen.
3. Listen to Your Body
It’s easy to get carried away, especially if swimming is something you love. However, if you feel any discomfort or pain around your incision, stop immediately and give your body more time to recover. Remember, there’s no rush.
4. Keep the Incision Dry Post-Swim
Once you’ve finished your swim, be sure to dry your incision area thoroughly. Pat the area gently with a clean towel, and avoid rubbing it. If you feel any unusual redness, swelling, or discharge, consult your doctor.
5. Stay Hydrated
Swimming can sometimes mask how much you’re sweating, so it’s important to stay hydrated. Drink plenty of water before and after your swim, especially if you’re still breastfeeding, as this can help with overall recovery and energy levels.
Alternative Activities Before Swimming
If you’re itching to get active but swimming isn’t an option yet, there are other gentle activities you can explore while waiting for your body to fully heal:
1. Walking
Walking is a safe and gentle way to increase your activity level after a C-section. Start with short distances and gradually increase as you feel more comfortable.
2. Pelvic Floor Exercises
Strengthening your pelvic floor muscles with exercises like Kegels can help improve core stability and support overall recovery.
3. Gentle Stretching
Incorporating light stretching can help ease tension and improve mobility. Just be mindful not to overstretch your abdominal area.
How to Know You’re Ready
Beyond the basic timeline, how can you tell you’re ready to swim after your C-section? Here are a few signs to look for:
– Pain-free incision: Your incision should no longer be tender, red, or swollen.
– No more bleeding: Lochia (postpartum bleeding) should have completely stopped. If you’re still spotting, it’s not yet time to swim.
– Comfort with daily activities: If you’re able to move around comfortably, lift light objects, and engage in basic physical activities without discomfort, you’re likely in a good place to start swimming.
The Bottom Line
Getting back into the water after a C-section is something many moms look forward to, but it’s crucial to wait until your body is fully healed. While the typical recovery time is 6-8 weeks, always consult your healthcare provider to ensure your individual recovery is on track before heading to the pool.
Swimming can be an excellent form of exercise for new moms, offering relaxation and gentle re-entry into physical activity, but taking the proper precautions is key. Remember, postpartum recovery is unique for every woman, so take it slow, be patient with yourself, and give your body the time it needs to heal fully.
So, when can you dive in? Once you’ve crossed that 6-8 week mark and have the all-clear from your doctor, go ahead and enjoy the water—but always with safety in mind!
Unlocking the 4 Types of PCOS: Which One Do You Have?

Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects up to 10% of women of reproductive age, and yet it’s often misunderstood. When most people think of PCOS, they picture symptoms like irregular periods, weight gain, and cysts on the ovaries, but PCOS is far more complex than that. Did you know that there are actually four different types of PCOS? Each type has its own causes, symptoms, and treatment approaches. So, how do you know which type of PCOS you have, and what can you do about it?
In this guide, we’ll break down the four main types of PCOS, explain how they differ, and help you figure out which type you might be dealing with. By understanding your specific PCOS type, you can tailor your approach to managing it and get back to feeling like your best self.
What Is PCOS?
Before we dive into the different types of PCOS, let’s quickly define what it is. PCOS is a hormonal disorder that disrupts the balance of reproductive hormones in women, causing a variety of symptoms. These include irregular periods, excess androgen levels (male hormones), insulin resistance, and small cysts on the ovaries. It’s one of the leading causes of infertility, but it can also affect your overall health, from your skin to your weight, and even your mood.
However, not all cases of PCOS are the same. That’s where the four types come in. Each type has its own root cause and requires a slightly different treatment plan. Let’s break it down.
The Four Types of PCOS
1. Insulin-Resistant PCOS
2. Post-Pill PCOS
3. Inflammatory PCOS
4. Adrenal PCOS
Let’s explore each type in more detail.
1. Insulin-Resistant PCOS (The Most Common Type)
Overview:
Insulin-resistant PCOS is by far the most common form of PCOS, and it’s driven by insulin resistance. In this type, your body struggles to use insulin effectively, which leads to higher levels of insulin circulating in the blood. These excess insulin levels stimulate the ovaries to produce more androgens (male hormones like testosterone), which can worsen PCOS symptoms like acne, excess facial hair, and irregular periods.
Key Symptoms:
– Weight gain, especially around the belly
– Difficulty losing weight
– Fatigue, particularly after eating
– Sugar cravings
– Dark patches of skin (acanthosis nigricans), often on the neck or underarms
Diagnosis:
Insulin resistance is diagnosed through blood tests, including fasting insulin and glucose levels. You may also have a glucose tolerance test.
Treatment:
– Dietary changes: a low-carbohydrate, low-sugar diet can help manage insulin resistance. Focus on whole foods like vegetables, lean protein, and healthy fats.
– Exercise: Regular physical activity, especially strength training and aerobic exercise, can improve insulin sensitivity.
– Medications: Doctors may prescribe metformina medication that helps the body use insulin more effectively.
If you’re struggling with stubborn weight gain or find yourself constantly craving sweets, you might have insulin-resistant PCOS. Fortunately, with the right lifestyle changes, this type can be well-managed.
2. Post-Pill PCOS (The Temporary Type)
Overview:
Post-pill PCOS occurs after stopping birth control pills, specifically those that suppress ovulation. When you stop taking the pill, your body may experience a temporary hormonal surge that can mimic PCOS symptoms. This type of PCOS is temporary and usually resolves on its own after a few months.
Key Symptoms:
– Irregular periods after stopping birth control
– Temporary acne flare-ups
– Slight increase in facial or body hair growth
Diagnosis:
Post-pill PCOS is often diagnosed when a woman who previously had regular periods before starting the pill develops PCOS-like symptoms after discontinuing it. It’s important to rule out other causes of PCOS first, such as insulin resistance or inflammation.
Treatment:
– Wait and see: Post-pill PCOS often resolves within 6-12 months as your hormones naturally balance out after stopping birth control.
– Support your body: Focus on supporting your body with balanced nutrition, stress management, and regular exercise.
– Natural supplements: Consider supplements that support hormone balance, like vitex (chasteberry) or magnesium.
This type of PCOS can be frustrating, but the good news is that it’s typically short-lived. If you’ve recently stopped taking birth control and noticed irregular cycles or acne, don’t panic. Give your body some time to adjust.
3. Inflammatory PCOS (The Immune System Type)
Overview:
Inflammatory PCOS is driven by chronic inflammation. When the body is under constant stress or battling inflammation, it can trigger excess androgen production, leading to PCOS symptoms. This type is often linked to poor gut health, food intolerances, stress, and environmental toxins.
Key Symptoms:
– Chronic fatigue
– Skin issues like eczema or psoriasis
– Digestive issues (bloating, IBS-like symptoms)
– Joint pain or aches
– Unexplained headaches
Diagnosis:
Inflammatory PCOS is often diagnosed based on symptoms and blood tests that measure markers of inflammation, such as C-reactive protein (CRP). Testing for food intolerances or gut health imbalances can also be helpful.
Treatment:
– Anti-inflammatory diet: Focus on reducing inflammation by eating whole, nutrient-dense foods. Add plenty of anti-inflammatory foods like fatty fish, leafy greens, turmeric, and ginger to your meals.
– Gut health support: Consider taking a probiotic supplement to support your gut health, which plays a major role in regulating inflammation.
– Stress management: Practices like yoga, meditation, or deep breathing can help reduce the chronic stress that often accompanies inflammatory PCOS.
If you constantly feel run-down or struggle with unexplained aches and pains, inflammation might be at the root of your PCOS. Treating the underlying inflammation can significantly improve your symptoms.
4. Adrenal PCOS (The Stress-Related Type)
Overview:
Adrenal PCOS is caused by an overproduction of androgens from the adrenal glands, rather than the ovaries. This type is often linked to chronic stress or trauma. Unlike other types of PCOS, women with adrenal PCOS typically have normal insulin levels and regular menstrual cycles, but they still experience elevated androgen symptoms.
Key Symptoms:
– Anxiety or feelings of being “on edge”
– Hair loss or thinning on the scalp
– Acne flare-ups, especially during stressful periods
– Difficulty sleeping
– High cortisol levels
Diagnosis:
Adrenal PCOS can be identified by testing your DHEA-S (a marker of adrenal androgen production) and cortisol levels. If DHEA-S is elevated but other androgens (like testosterone) are normal, adrenal PCOS may be the culprit.
Treatment:
– Stress management: Reducing stress is critical for managing adrenal PCOS. Incorporate relaxation techniques like yoga, meditation, and breathing exercises into your routine.
– Sleep: Prioritize getting 7-9 hours of quality sleep each night, as poor sleep can exacerbate adrenal imbalances.
– Supplements: Consider taking adaptogens (like ashwagandha or rhodiola) to support adrenal function and reduce cortisol levels.
If you tend to experience PCOS symptoms primarily during stressful times, adrenal PCOS may be your type. Learning to manage stress and support your adrenal glands can make a huge difference in your symptoms.
Which Type of PCOS Do You Have?
Now that you know about the four types of PCOS, you may be wondering which type applies to you. It’s possible to have characteristics of more than one type, so it’s important to work with a healthcare provider or fertility specialist to get a proper diagnosis.
Here are some steps you can take:
– Track your symptoms: Keep a journal of your symptoms, menstrual cycles, and any lifestyle factors that might influence them.
– Consult your doctor:Talk to your healthcare provider about getting the necessary blood tests to determine which type of PCOS you have. They can measure hormones, insulin levels, and inflammation markers to help pinpoint the cause.
– Tailor your treatment: Once you know your type, you can customize your diet, supplements, and lifestyle changes to better manage your specific symptoms.
The Bottom Line
PCOS is a multifaceted condition, but understanding your specific type can make all the difference when it comes to managing your symptoms and improving your quality of life. Whether you’re dealing with insulin resistance, post-pill hormonal imbalance, chronic inflammation, or adrenal stress, there are targeted steps you can take to support your body and regain balance.
By focusing on your unique needs, you’ll be one step closer to unlocking the key to managing your PCOS and living your healthiest life. So, which type do you think you have? It’s time to take charge of your health and find the solution that works best for you!
Relieve SPD Pain: Top Exercises for Symphysis Pubis Dysfunction Relief

If you’re dealing with Symphysis Pubis Dysfunction (SPD), you know how challenging it can be to navigate everyday life. Whether it’s standing, walking, or even just rolling over in bed, the discomfort and pain can really get in the way. But don’t worry—you’re not alone, and there are exercises specifically designed to help relieve that pesky SPD pain and improve your overall pelvic stability.
In this article, we’ll dive into what SPD is, why it happens (especially during pregnancy), and the best exercises to help manage and reduce your symptoms. With a little movement and the right techniques, you’ll be on your way to feeling more comfortable and confident in no time.
What is Symphysis Pubis Dysfunction (SPD)?
Symphysis Pubis Dysfunction, also known as Pelvic Girdle Pain (PGP), occurs when the ligaments that normally keep your pelvic bones aligned become too relaxed and stretchy, causing pain in the pelvic region. This is particularly common during pregnancy due to the hormone relaxin, which helps the body prepare for childbirth by loosening the joints and ligaments in the pelvis.
The symphysis pubis is the joint located at the front of your pelvis where the two pubic bones meet. When this joint becomes too relaxed, it can lead to misalignment and pain in the lower pelvis, hips, lower back, and even down the legs.
Common Symptoms of SPD
– Pain in the pubic area: A sharp or stabbing sensation that worsens with movement.
– Lower back pain: Especially around the sacroiliac joints.
– Difficulty walking: You may notice a waddling gait or pain when lifting one leg.
– Hip discomfort: SPD can make it painful to perform actions like getting out of bed, climbing stairs, or even standing on one leg.
– Clicking or grinding sensation: You might feel or hear a clicking sound in your pelvic area when moving.
Why Does SPD Happen, and Who’s at Risk?
SPD most commonly occurs during pregnancy due to the body’s preparation for childbirth, but it can also affect non-pregnant individuals, particularly athletes or those with hypermobility.
Pregnancy-related SPD is often triggered by:
– Hormonal changes: The hormone relaxin softens the ligaments and joints in the pelvic region, causing instability.
– Previous pelvic injury: Women who have had pelvic trauma or injury before pregnancy are more prone to developing SPD.
– Multiple pregnancies: Each subsequent pregnancy increases the likelihood of SPD.
Now that we understand what SPD is and why it happens, let’s get into the good stuff— exercises that can help relieve your pain and discomfort.
Top Exercises to Relieve SPD Pain
These exercises focus on strengthening the muscles around your pelvis, hips, and lower back, providing greater stability to the area and helping to ease the pain caused by SPD. Remember, it’s important to start slow and listen to your body. If any exercise increases your pain, stop immediately and consult your healthcare provider.
1. Pelvic Tilts
Pelvic tilts are a gentle exercise that strengthens your abdominal muscles and supports your pelvis.
How to do it:
– Start by lying on your back with your knees bent and feet flat on the floor. Place your hands on your hips.
– Gently flatten your back against the floor by tilting your pelvis upwards, engaging your abdominal muscles.
– Hold this position for a few seconds, then slowly release back to neutral.
– Repeat 10-12 times.
Tip: If lying on your back is uncomfortable during pregnancy, you can perform pelvic tilts while standing against a wall or on all fours.
2. Kegels
Kegels strengthen your pelvic floor muscles, which can help stabilize your pelvis and reduce the pain associated with SPD.
How to do it:
– Sit, stand, or lie down in a comfortable position.
– Squeeze your pelvic floor muscles as if you’re trying to stop the flow of urine.
– Hold the squeeze for 5 seconds, then relax.
– Repeat 10-15 times, gradually increasing the hold time as your strength improves.
Tip: If you’re not sure how to engage your pelvic floor, try practicing Kegels while using the restroom by stopping your flow of urine mid-stream. (But don’t do this regularly as it can weaken your muscles over time.)
3. Hip Squeeze (With a Ball or Pillow)
This exercise strengthens the inner thighs and pelvic muscles, which can help stabilize your pubic symphysis.
How to do it:
– Sit or lie down on your back with your knees bent and feet flat on the floor.
– Place a small ball or pillow between your knees.
– Squeeze the ball or pillow by bringing your knees together, holding the tension for 5-10 seconds.
– Release and repeat 10-12 times.
Tip:You can also do this exercise in a seated position if lying down is uncomfortable.
4. Cat-Cow Stretch
The Cat-Cow stretch is a gentle way to mobilize the spine and pelvis, helping to relieve tension in your lower back and pelvic area.
How to do it:
– Get on your hands and knees in a tabletop position.
– As you inhale, arch your back, allowing your belly to drop towards the floor (Cow pose).
– As you exhale, round your back, tucking your chin towards your chest and pulling your belly button towards your spine (Cat pose).
– Repeat this movement slowly 8-10 times, focusing on smooth transitions between the two poses.
Tip: This is a great stretch to do during pregnancy, as it helps alleviate lower back pain and keeps the spine flexible.
5. Bridge Pose
The bridge pose helps strengthen the glutes, lower back, and core, which are all essential for pelvic stability.
How to do it:
– Lie on your back with your knees bent and feet hip-width apart.
– Slowly lift your hips off the ground, pressing through your feet and squeezing your glutes.
– Hold the bridge position for 5-10 seconds, then lower your hips back down.
– Repeat 10-12 times.
Tip:Keep your core engaged to avoid straining your lower back. You can also place a pillow or yoga block under your hips for added support if needed.
6. Modified Side Plank
Side planks strengthen your obliques and the muscles around your hips and pelvis, which can help with SPD pain.
How to do it:
– Lie on your side with your knees bent, and prop yourself up on your forearm.
– Lift your hips off the ground, creating a straight line from your shoulders to your knees.
– Hold for 10-20 seconds, then lower back down.
– Repeat on the other side.
Tip:If you feel unstable, keep your bottom leg bent for extra support. As your strength improves, you can straighten both legs for a more challenging variation.
7.Swimming
Swimming is one of the best exercises for SPD because it’s low-impact and helps reduce pressure on your pelvis. The water supports your body weight, allowing you to move more freely without aggravating your symptoms.
How to do it:
– Try swimming gentle laps, focusing on smooth, controlled movements.
– Avoid breaststroke, as the leg movements can exacerbate pelvic pain.
– Water aerobics can also be a great option for maintaining fitness without putting strain on your pelvis.
Tip: If you’re new to swimming or don’t feel confident, consider using a kickboard or pool noodle for support.
Additional Tips for Managing SPD
In addition to regular exercise, here are a few extra tips to help you manage SPD:
1. Wear a pelvic support belt: A maternity or pelvic support belt can help stabilize your pelvis and reduce pain during daily activities.
2. Modify your movements: When standing, keep your weight evenly distributed on both feet. Avoid putting all your weight on one leg or twisting your body too much.
3. Take breaks: If you have to stand or walk for long periods, make sure to rest frequently and avoid over-exerting yourself.
4. Sleep with a pillow between your knees: Keeping your legs aligned while sleeping on your side can reduce strain on your pelvis.
5. Talk to a physical therapist: If your SPD pain is severe, consider seeing a physical therapist who specializes in pelvic health. They can create a tailored exercise plan and offer hands-on treatments to relieve your discomfort.
The Bottom Line
Dealing with Symphysis Pubis Dysfunction can be tough, but incorporating gentle exercises into your daily routine can make a big difference in managing pain and improving your mobility. Focus on strengthening the muscles around your pelvis, practicing good posture, and making small adjustments to your movements to protect your pelvic area.
If you’re ever unsure whether an exercise is right for you or if your pain worsens, always consult your healthcare provider for personalized advice. With the right exercises and support, you can find relief and get back to feeling more comfortable in your body.
Give these exercises a try, stay consistent, and soon you’ll be well on your way to relieving SPD pain and improving your overall pelvic health!
Top Tips for a Successful IUI: Your Ultimate Guide to Boosting Success

If you're on a fertility journey, chances are you’ve heard of IUI (Intrauterine Insemination). It's one of the most common fertility treatments, often used as a stepping stone before considering more advanced procedures like IVF. But even though it's a less invasive and more affordable option, it's natural to want to give yourself the best chance at success. So, what can you do to boost the odds? This guide will walk you through everything you need to know about IUI and share top tips for increasing your chances of a successful outcome.
What Is IUI, and How Does It Work?
Let’s start with the basics. IUI, or intrauterine insemination, is a fertility treatment that involves placing sperm directly into a woman's uterus around the time of ovulation. The goal is simple: to bring sperm closer to the egg, making fertilization easier. For couples dealing with issues like low sperm count, mild male infertility, unexplained infertility, or ovulation problems, IUI can significantly enhance the chances of conception.
The process itself is straightforward:
1. Ovulation is tracked, sometimes with the help of medications.
2. At the right time, sperm (from a partner or a donor) is processed and concentrated in a lab.
3. A doctor uses a small catheter to insert the sperm into the uterus, bypassing the cervix and giving it a head start toward the egg.
While IUI is a less invasive fertility treatment, it still involves some crucial factors that can influence its success. Here’s a breakdown of the top tips and steps you can take to improve your chances of success during the IUI process.
Timing is everything with IUI. The procedure must be done during the woman’s ovulation window to maximize the chances of fertilization. Ovulation typically occurs around the middle of your menstrual cycle, but every woman’s cycle is different.
Here’s how you can accurately track your ovulation:
– Ovulation Predictor Kits (OPKs): These at-home urine tests detect the surge of luteinizing hormone (LH) that happens right before ovulation. Once you get a positive result, IUI is typically scheduled within 24-36 hours.
– Ultrasound Monitoring: Many fertility clinics use ultrasounds to track the growth of follicles in the ovaries, helping doctors pinpoint the exact time of ovulation.
– Basal Body Temperature: Although less precise, tracking your basal body temperature daily can help indicate when ovulation is occurring.
By ensuring the IUI procedure is performed at the optimal time, you significantly increase the likelihood of sperm meeting the egg.
2. Medications Can Improve Success Rates
In many cases, doctors will prescribe medications to stimulate ovulation or improve egg quality. Medications can also help regulate your cycle if it's irregular. Common fertility medications used in IUI treatments include:
– Clomid (Clomiphene Citrate): Often the first choice, Clomid is an oral medication that helps stimulate ovulation.
– Letrozole (Femara): Another oral medication that can stimulate ovulation, Letrozole is sometimes used for women who don’t respond to Clomid.
– Gonadotropins: These injectable hormones stimulate the ovaries to produce multiple eggs, increasing the chances of success. However, they come with a higher risk of multiple pregnancies (twins or more).
Working with your fertility specialist to develop a medication plan tailored to your body and cycle can improve IUI success rates. Just be sure to monitor your body’s response closely to avoid complications like ovarian hyperstimulation syndrome (OHSS).
3. Focus on Sperm Quality
Whether you’re using your partner’s sperm or donor sperm, quality matters. The higher the count of healthy, motile sperm, the better the chances of fertilization. Here are some ways to optimize sperm quality for the procedure:
– Healthy Diet: Encourage your partner to focus on a diet rich in antioxidants, which can improve sperm quality. Foods like berries, nuts, leafy greens, and fish are all packed with nutrients that support reproductive health.
– Supplements: Certain vitamins and minerals, such as vitamin C, vitamin E, zinc, and folic acid, may improve sperm health. Many men take fertility supplements that combine these essential nutrients.
– Avoid Heat: Heat can lower sperm count, so avoiding hot tubs, saunas, and keeping laptops off laps is recommended.
– Cut Back on Alcohol and Smoking: Excessive alcohol and smoking are known to negatively impact sperm health. Cutting back or eliminating these habits can improve outcomes.
If sperm quality is a concern, you may want to discuss additional testing with your fertility specialist. In some cases, advanced sperm selection techniques, such as ICSI (intracytoplasmic sperm injection), may be considered.
4. Maintain a Healthy Lifestyle
Your overall health can have a direct impact on fertility, so it’s essential to prioritize a balanced, healthy lifestyle leading up to your IUI procedure.
– Exercise Regularly: Moderate exercise can help regulate your menstrual cycle and boost fertility. However, avoid intense workouts, which may disrupt ovulation.
– Eat a Nutrient-Dense Diet: Focus on a diet rich in fruits, vegetables, whole grains, and lean proteins. The Mediterranean diet, in particular, has been linked to improved fertility outcomes.
– Stay Hydrated: Proper hydration supports overall bodily functions, including reproductive health.
– Manage Stress:Stress can disrupt hormone balance and ovulation. Incorporate relaxation techniques such as meditation, yoga, or deep breathing exercises to manage stress levels throughout your fertility journey.
5. Mind Your Weight
Both being underweight and overweight can negatively impact your fertility. Studies show that women with a Body Mass Index (BMI) in the normal range (18.5-24.9) tend to have higher success rates with IUI.
– Underweight: If your BMI is too low, it may disrupt your hormone levels and stop ovulation altogether.
– Overweight: Excess weight can lead to hormonal imbalances, making it harder to conceive.
Working with a fertility nutritionist or healthcare provider to achieve a healthy BMI can be beneficial for improving your chances of conception through IUI.
6. Consider Acupuncture
Acupuncture is becoming an increasingly popular complementary treatment for women undergoing fertility treatments like IUI. While research on its efficacy is ongoing, some studies suggest that acupuncture can help improve blood flow to the reproductive organs, reduce stress, and support hormonal balance.
Consider working with a fertility-focused acupuncturist to see if this option might be right for you.
7. Stay Patient and Positive
It’s important to remember that, like any fertility treatment, IUI doesn’t always work on the first try. The success rate of IUI can vary depending on factors like age, underlying fertility issues, and overall health. Typically, IUI success rates range from 10-20% per cycle, but many women undergo 3-6 cycles before achieving pregnancy.
Staying patient and maintaining a positive outlook during the process can make all the difference. While it’s natural to feel a bit of stress or anxiety, try to focus on self-care and the steps you’re taking to improve your chances.
8. Consult Your Doctor Regularly
Ultimately, the most important tip for a successful IUI is maintaining close communication with your fertility specialist. Your doctor can tailor your treatment plan, adjust medications as needed, and ensure that all steps are optimized for your unique situation.
Don’t hesitate to ask questions, seek advice, and discuss any concerns with your healthcare team. They are there to support you every step of the way!
The Bottom Line
When it comes to IUI, there’s no magic formula for guaranteed success, but there are many ways to improve your odds. By focusing on timing, sperm quality, a healthy lifestyle, and regular communication with your doctor, you’ll put yourself in the best possible position to conceive. Patience is key, and every step you take brings you closer to your goal.
With these tips, you’re well-equipped to embark on your IUI journey with confidence. Whether it takes one cycle or several, stay hopeful and trust in the process—your little miracle could be just around the corner!
Unlocking Potential: Early Child Development and Its Impact

Early childhood is a remarkable period of growth and learning, where young minds are like sponges, soaking up knowledge and experiences that shape their future. It is during this critical time that children’s brains are developing at an astonishing rate, laying the foundation for their cognitive, social, emotional, and physical development.
The importance of early child development and its profound impact on a child’s lifelong journey
1. Cognitive Development in Early Childhood
From the moment children are born, their brains are wired to absorb information from their surroundings. Stimulating environments, rich with language, play, and exploration, provide the necessary building blocks for cognitive development. Through engaging activities, children develop cognitive skills such as memory, problem-solving, attention span, and language acquisition, setting the stage for future academic success.
2. Social and Emotional Development
Early childhood is the time when children begin to form their sense of self and start building relationships with others. Positive and nurturing interactions with parents, caregivers, and peers help children develop vital social and emotional skills. These skills include empathy, self-regulation, communication, and the ability to navigate and solve conflicts. A strong foundation in social and emotional development lays the groundwork for healthy relationships, resilience, and emotional well-being in later life.
3. Physical Development in Early Childhood
Early childhood is also a crucial period for physical development. Gross and fine motor skills, such as crawling, walking, and grasping objects, are refined and strengthened during this time. Physical activity and opportunities for outdoor play promote healthy growth, coordination, and gross motor skill development. Additionally, proper nutrition and healthcare contribute to overall physical well-being and support optimal growth and development.
4. Lifelong Learning and Success
The impact of early child development extends far beyond the early years. Research shows that children who receive a strong foundation in their early years perform better academically, have higher graduation rates, and experience greater success in adulthood. Early experiences shape the architecture of the brain, with lasting effects on learning, behavior, and health throughout a person’s lifespan.
5. Parental Involvement and Support
Parents play a crucial role in fostering their child’s early development. Engaging in warm and responsive caregiving, providing a stimulating learning environment, and being actively involved in a child’s development can have a profound impact on their growth and well-being. Seeking out resources, attending parenting programs, and connecting with supportive networks can empower parents to optimize their child’s early development.
Conclusion
Early child development is a window of opportunity to nurture and shape a child’s future. By prioritizing cognitive, social, emotional, and physical development in the early years, we unlock the potential of each child, setting them on a path towards lifelong learning and success. Let us embrace the responsibility to provide rich and nurturing experiences in these crucial years, empowering young minds to thrive and contribute positively to our world. Together, we can create a brighter future, one child at a time.
Women’s Health and Artificial Intelligence (AI)
Women’s Health and Innovation Summit (WHIS) – Boston September 2024
We recently attended the WHIS and were very impressed with the presentations particularly in the area of AI. AI is a game changer for the future of Women’s health. I have put some additional material together below. Many of the attendee’s were involved with start-ups utilising AI, particularly applications associated with imaging, where AI improves the Signal to Noise ratio and enhances the image to provide early detection and treatment for conditions such as endometriosis.
Artificial Intelligence (AI) in Women’s Health: A New Era of Personalized Medicine
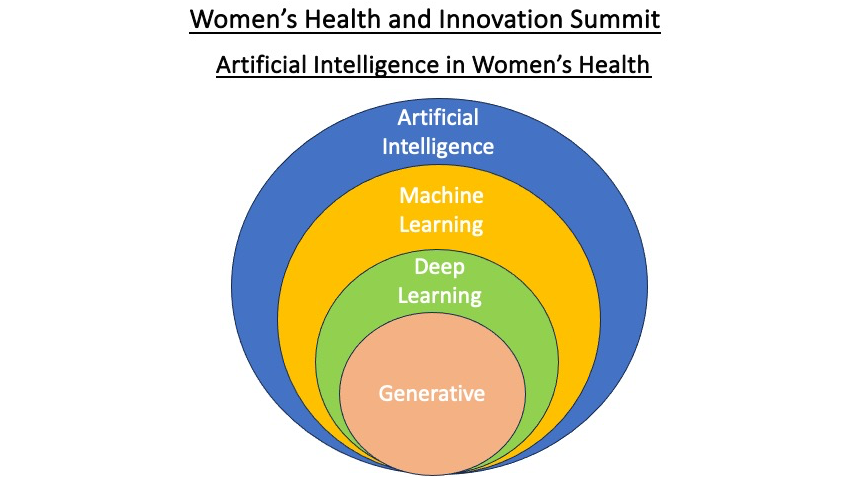
Artificial Intelligence (AI) is transforming the healthcare landscape, making it more precise, personalized, and accessible. By leveraging advanced algorithms, machine learning, and data analytics, AI empowers healthcare professionals with tools that improve diagnostics, treatment, and patient care outcomes. For women’s health, AI offers promising applications that can address specific medical needs, enhance early detection, and optimize health management across various stages of life.
What is AI in Healthcare?
AI refers to the use of computer systems that mimic human intelligence to process complex data and make decisions. In healthcare, AI technologies analyze medical data, assist in diagnosis, predict outcomes, and even recommend treatments based on individual patient profiles. AI’s ability to learn from vast amounts of data makes it especially powerful in detecting patterns that may not be visible to the human eye.
Key Applications of AI in Women’s Health
1. Early Detection and Diagnostics
AI is advancing early detection for diseases that disproportionately affect women, such as breast cancer, ovarian cancer, and cervical cancer. AI-powered systems can:
- Enhance mammography screening accuracy by identifying subtle patterns in imaging that human radiologists may miss, reducing false positives and negatives.
- Predict genetic risks for diseases like breast cancer using AI tools that analyze genetic data, allowing for preventive interventions.
- Screen cervical cancer through automated analysis of Pap smear images, enabling faster and more accurate diagnosis in resource-limited settings.
2. Personalized Medicine
Women’s health is uniquely influenced by hormonal cycles, pregnancy, menopause, and other gender-specific factors. AI can:
- Analyze genetic, hormonal, and lifestyle data to offer personalized treatment plans for conditions such as endometriosis, PCOS (polycystic ovary syndrome), and reproductive health.
- Support fertility treatments by predicting optimal times for conception or by improving the outcomes of procedures like IVF (in vitro fertilization) using predictive models.
3. Mental Health and Wellness
AI-powered chatbots and mental health applications are providing women with accessible mental health support, especially for conditions like postpartum depression, anxiety, and stress. These tools offer:
- Real-time emotional support via AI-driven platforms that can assess mood changes, track mental health trends, and provide early intervention.
- Personalized wellness recommendations tailored to an individual's psychological profile and needs.
4. Remote Monitoring and Telemedicine
AI facilitates remote monitoring of women’s health during pregnancy, chronic disease management, and post-surgical recovery. Wearables, combined with AI, can track vital signs, detect abnormalities, and alert healthcare providers to potential risks. For example:
- Gestational diabetes or preeclampsia can be monitored through AI-enabled wearable devices, ensuring timely interventions that can save lives.
- Telemedicine platforms use AI to triage symptoms and provide faster access to care, especially for women in rural or underserved areas.
Addressing Inequities in Women’s Health Through AI
Despite advances in healthcare, women often face disparities in treatment and diagnosis. AI holds the potential to bridge these gaps by:
- Improving access to care for marginalized women who may lack access to specialist care through AI-powered telehealth services.
- Eliminating biases in research and care by training AI systems on diverse datasets that represent women of different ethnicities, ages, and socioeconomic backgrounds. This ensures that treatment algorithms are equitable and effective for all women.
The Future of AI in Women’s Health
As AI continues to evolve, its applications in women’s health will expand. From predictive analytics that forewarn of complications during pregnancy to virtual assistants that guide women through menopause, AI is shaping a future of healthcare that is more responsive, personalized, and preventative.
For women, this means more empowered health decisions, earlier interventions, and a greater understanding of their bodies across all stages of life. The partnership between women’s health experts and AI technologies can create a healthcare ecosystem that prioritizes precision care, equity, and accessibility for all.
This intersection of AI and women’s health marks a significant step toward a new era of healthcare, where technology empowers women to live healthier, more informed lives. The future is bright, and AI is paving the way.
We look forward to WHIS September 2025, as we are certain AI applications will have advanced dramatically by this time.
“Men’s Role in Pregnancy: Understanding Their Involvement”

The Vital Role of Men in Pregnancy: Nurturing Support and Partnership.
Pregnancy is an incredible journey that not only impacts the expectant mother but also involves the crucial participation of men. While it’s undeniable that women experience physical changes and bear the child, men play an essential role in providing emotional support, being actively involved in decision-making, and creating a nurturing environment for their partner. In this article, we will explore the significant ways in which men can contribute during pregnancy and how their involvement positively impacts the overall experience.
1. Emotional Support:
During pregnancy, women undergo numerous emotional and hormonal changes, which can sometimes be overwhelming. Men can provide a strong pillar of support by being understanding, patient, and empathetic. Listening attentively, offering a shoulder to lean on, and engaging in open and honest communication can help foster emotional well-being for both partners.
2. Attending Medical Appointments:
Accompanying your partner to prenatal check-ups and ultrasound appointments demonstrates your commitment and involvement. It allows you to witness the growth of your baby firsthand and enables you to ask questions and gain a deeper understanding of the pregnancy process. This active participation will strengthen the bond between you, your partner, and your growing family.
3. Education and Research:
Take the initiative to educate yourself about the various stages of pregnancy, common symptoms, and potential complications. By being well-informed, you can provide reassurance, answer questions, and offer guidance to your partner. Researching together can also be an excellent bonding opportunity as you prepare for the arrival of your little one.
4. Healthy Lifestyle Choices:
Supporting your partner in maintaining a healthy lifestyle is crucial for her well-being and the baby’s development. Encourage nutritious eating habits, engage in regular exercise together (if approved by a healthcare professional), and avoid harmful substances such as alcohol and tobacco. These choices promote a healthy pregnancy and set the stage for a positive start to parenthood.
5. Creating a Nurturing Environment:
Transform your home into a haven of comfort and safety. Help with organizing the nursery, assembling furniture, and ensuring that everything is baby-proofed. By actively participating in these preparations, you show your commitment and readiness to embrace the new role of fatherhood.
6. Parenting Classes:
Attending parenting classes together can provide invaluable knowledge and skills for both partners. Learning about newborn care, breastfeeding, and infant CPR equips you with the tools needed to confidently navigate the early stages of parenthood. Additionally, these classes offer an opportunity to connect with other expectant couples and share experiences.
Pregnancy is a beautiful journey that calls for the joint effort and dedication of both parents. Men have a unique opportunity to actively participate, offering emotional support, attending medical appointments, and engaging in various preparations. By taking an active role in pregnancy, men contribute to creating a nurturing environment and establishing a foundation of partnership and teamwork. Embrace this incredible opportunity to be an involved and supportive partner, and witness the transformative power of your presence throughout the journey of pregnancy and beyond.
Sistapedia® & Women’s Health Innovation Summit – Boston 2024

Women’s Health and Innovation Summit (WHIS) – Boston 2024
Earlier this month I attended the WHIS in Boston. The summit was over three days and packed full of new ideas, and innovative solutions to problems in women’s health.
Sources of information on the key problems in Women’s Health:
- Closing the Women’s Health Gap: McKinsey Insight Report 2024;
- Gates Foundation, Women’s Health Innovation Opportunity Map 2023;
- White House Initiative on Women’s Health Research 2023.
Some problem examples:
-
- Endometrioses is on the rise and very difficult to detect and diagnose, leaving many women in excruciating pain from unknow sources. It is estimated that the world market for solutions is in excess of $250B giving an indication of the size of this problem.
Fortunately, many of the innovations being developed by start-up companies are targeting this area. Solutions include MRI image resolutions < 5mm with some reports of the possibility of < 1mm. The current state of the art is resolutions > 5mm.
Another approach is an injectable substance that results in the enhanced image of tumours allowing < 1mm image resolution.
Unfortunately the FDA approval process of treatments results in long lead times getting solutions to market; typically a > 5-year process.
-
- Unexplained deaths in childbirth and in the post-natal period by minority races such as, African Americans, Asians and Latin Americans. The data is not very rich in this area, but the lesson being learned is that each woman can have unique treatment / care requirements, and that a one approach fits all is not appropriate.
- Women are more likely to die from a heart attack than a man; they are often misdiagnosed and discharged from hospital only to die shortly after. The observation here is that women are getting the same treatment as men despite their very different physiology.
- Women are 80% more likely to suffer from an auto immune disease, such as, diabetes than a man.
- Women in general throughout their lives suffer 25% more debilitating illness than men, with PMS being a major contributor. A common myth is that because women generally live longer, then they are healthier than men; the data indicates this myth is false.
Some non-health related causes to the lack of action in addressing health issues associated with women, are as follows:
- There is a significant lack of representation of women in industry at middle and upper management levels, in companies dealing with specific women’s health issues.
- Only about 2% of Venture Capital companies have been investing in companies / start-ups involving women led companies addressing women specific health issues.
- It is only since 2018 that we have started to see women founders in predominantly women led companies, addressing women’s health issues.
- A glaring anomaly is that women led start-up companies are 68% more successful than start-up companies led by men.
- To confuse this issue even further women are 51% of the US population; women are responsible for 80% of a family’s financial decisions and the global women’s health market is in the trillions of dollars.
- Research on the human body is primarily based on the male anatomy and then applied to women. Incredible as this sounds it is true. I recently read Bill Bryson’s book, The Human Body, which also revealed this anomaly.
- For every $1 invested in women’s health, $3 is generated in the economy.
A great outcome for me was the confirmation of the importance of Sistapedia® in addressing many of the issues highlighted in the following reports:
- Closing the Women’s Health Gap: McKinsey Insight Report 2024;
Gates Foundation, Women’s Health Innovation Opportunity Map 2023;
- White House Initiative on Women’s Health Research 2023.
Sistapedia® addresses the equity and access to information and resource issues in the above reports, as follows:
- Allows all women (Sistas) free access to information and resources relating to women’s health, through the Sistapedia.com website;
- Provides a trusted environment for all women wishing to be verified for free at Sistapedia.com;
Note: Sistas choosing not to be verified are still permitted access to information and resources, but will lack credibility to other Sistas and Providers / Specialist / Health Care Practitioners.
- Provides verified sources of information from Service and Product suppliers, as well as Medical Specialist and Health Care Practitioners.
So following this summit we need to get the message of Sistapedia® out there and start addressing the issues raised.
