Tag: IVF
“Discover the Miraculous Benefits of Surrogacy for Parents”

Surrogacy: A Life-Changing Journey Bringing Miracles to Aspiring Parents
In today’s fast-paced world, the beauty of surrogacy is unfolding as a miraculous solution for aspiring parents yearning to the joy of parenthood. Surrogacy offers a glimmer of hope, a ray of light, and a profound opportunity for couples facing fertility challenges. This article will delve into the mesmerizing world of surrogacy, exploring numerous benefits of surrogacy and why it has become a beacon of hope for parents-to-be worldwide.
1. Embracing the Miracle of Surrogacy
Surrogacy is an extraordinary process where a compassionate woman selflessly carries and nurtures a child for another couple or individual. It is a journey that defies limits, transcending biological barriers, and offering a pathway to parenthood where all hope seemed lost. The willingness of surrogate mothers to help create families is truly awe-inspiring, making surrogacy a remarkable and life-changing experience.
2. A Solution for Fertility Challenges
For couples grappling with infertility issues, surrogacy provides a glimmer of hope. Whether it is due to medical conditions, genetic concerns, or other factors, surrogacy allows individuals to overcome these obstacles and fulfill their dreams of becoming parents. With the advancements in reproductive technology, surrogacy has become a viable option for couples who may have once felt defeated by their circumstances.
3. Tailored to Individual Needs
One of the significant advantages of surrogacy is its versatility. It caters to various situations, offering both traditional and gestational surrogacy options. In traditional surrogacy, the surrogate mother uses her own eggs, while gestational surrogacy involves the use of assisted reproductive technologies, where the embryo is created using the intended parents’ genetic material. This flexibility ensures that aspiring parents can choose the surrogacy method that aligns best with their preferences and needs.
4. Emotional Support and Guidance
Surrogacy agencies and professionals play a vital role in supporting aspiring parents throughout their surrogacy journey. These experts provide emotional support, guidance, and legal assistance, ensuring a smooth and transparent process. From matching intended parents with suitable surrogates to navigating legal complexities, their expertise eases the emotional burden and provides a solid foundation for a successful surrogacy experience.
5. Global Accessibility
Surrogacy is no longer confined to a few countries or regions. Thanks to globalization and increasing awareness, aspiring parents can explore surrogacy options worldwide. Countries like the United States, Ukraine, and Canada have gained recognition for their well-regulated and supportive surrogacy programs. This global accessibility broadens the horizons for individuals seeking surrogacy as a viable solution, offering them the chance to embark on this life-changing journey.
Surrogacy is undeniably a miraculous and awe-inspiring avenue for parents-to-be. It brings hope, joy, and fulfillment to those who have faced fertility challenges. With its countless benefits, surrogacy provides a beacon of light, offering individuals the opportunity to experience the miracle of parenthood. Whether it’s the bond between intended parents and surrogate mothers or the emotional support provided by surrogacy professionals, this journey is a testament to the resilience and compassion of humanity. Surrogacy truly stands as a transformative option, bringing miracles to aspiring parents worldwide.
In-Vitro Maturation (IVM): Assisted Reproductive Technology
In-Vitro Maturation (IVM) is a groundbreaking technique in the field of assisted reproductive technology (ART) that offers hope to individuals and couples struggling with fertility issues. Unlike traditional in-vitro fertilization (IVF), which requires the use of fertility medications to stimulate the ovaries, IVM involves the retrieval and maturation of immature eggs from the ovaries. In this article, we will explore the concept of In-Vitro Maturation, its advantages and limitations, and its potential as a fertility treatment option.
Understanding In-Vitro Maturation (IVM)
In-Vitro Maturation (IVM) is an alternative approach to traditional IVF that involves the collection and maturation of immature eggs (oocytes) from the ovaries outside of the body. Unlike IVF, where fertility medications are used to stimulate the ovaries to produce multiple mature eggs, IVM allows for the collection of immature eggs that can be matured in the laboratory setting.
The IVM Process
The IVM process typically involves the following steps:
1. Ovarian Stimulation
In some cases, mild ovarian stimulation may be performed using low doses of fertility medications to encourage the growth of multiple follicles in the ovaries. However, in most IVM cycles, little to no ovarian stimulation is used.
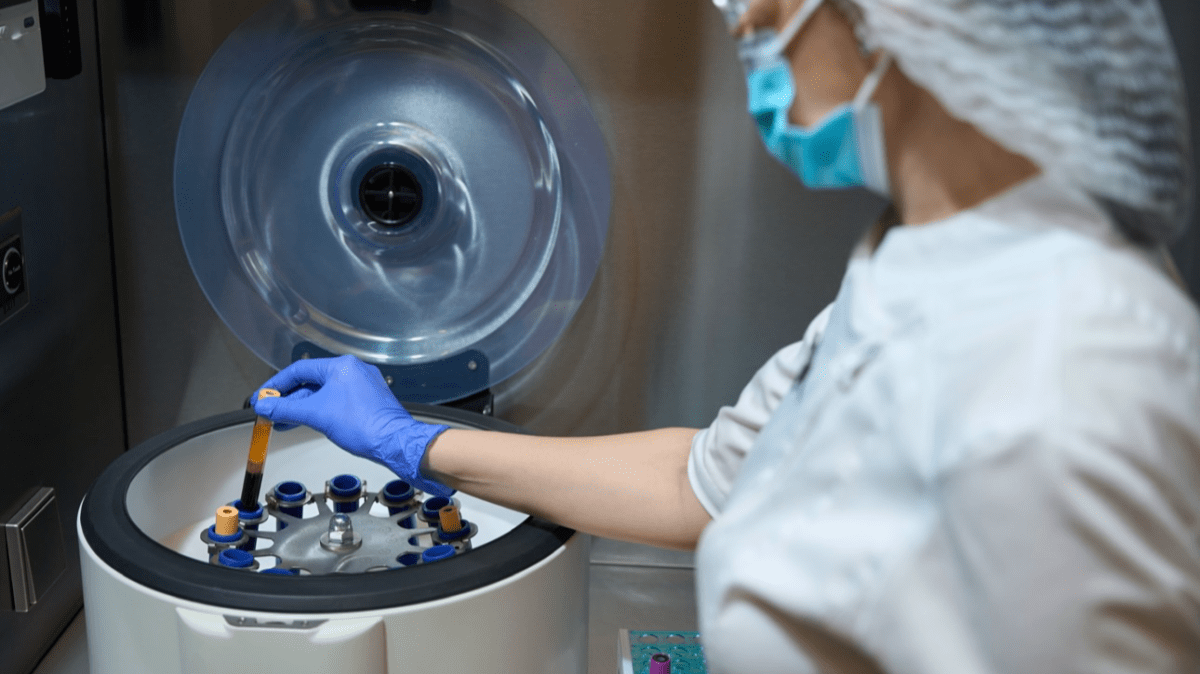
2. Egg Retrieval
Using ultrasound guidance, the retrieval of immature eggs from the ovaries is done through a needle aspiration procedure. This is usually done under local anesthesia or mild sedation.
3. Laboratory Maturation
The retrieved immature eggs are then placed in a culture medium in the laboratory, where they are allowed to mature over a period of 24 to 48 hours. During this time, the eggs undergo the necessary changes required for fertilization.
4. Fertilization
After the maturation of eggs, they undergo fertilization using conventional IVF techniques. This involves combining the mature eggs with sperm in the laboratory to facilitate fertilization.
5. Embryo Transfer
After fertilization, the resulting embryos are monitored for development and quality. The most viable embryos are selected for transfer into the uterus, while any remaining embryos may be cryopreserved for future use.
Advantages of In-Vitro Maturation (IVM)
1. Reduced Need for Ovarian Stimulation
Unlike traditional IVF, IVM requires little to no ovarian stimulation. This reduces the risk of ovarian hyperstimulation syndrome (OHSS), a potential complication associated with IVF treatment.
2. Time and Cost Efficiency
IVM treatment is often shorter and less expensive than traditional IVF since it eliminates or reduces the need for fertility medications and frequent monitoring.
3. Suitable for Certain Patient Groups:
IVM may be a suitable option for individuals who are at risk of complications from ovarian stimulation, such as those with polycystic ovary syndrome (PCOS) or a high risk of OHSS.
4. Ethical Considerations
Some individuals may prefer IVM due to ethical concerns associated with the use of fertility medications or concerns about potential multiple pregnancies.
Limitations and Considerations of In-Vitro Maturation (IVM)
1. Lower Success Rates
Compared to traditional IVF, IVM may have lower success rates, especially in cases where the eggs retrieved are of lower quality or maturity.
2. Limited Availability
IVM is a specialized technique that may not be widely available at all fertility clinics. Individuals interested in pursuing IVM may need to research and locate a clinic that offers this specific treatment option.
3. Fewer Eggs Retrieved
In IVM, typically fewer eggs are retrieved compared to traditional IVF. This may limit the number of embryos available for transfer and potentially decrease the chances of success.
4. Need for Additional Research
From further research, we can fully understand the long-term outcomes and success rates of IVM in comparison to traditional IVF.
Is IVM Right for You?
Determining whether IVM is the right treatment option depends on various factors, including your specific fertility diagnosis, age, and individual preferences. It is essential to consult with a fertility specialist or reproductive endocrinologist who can evaluate your unique circumstances and provide personalized recommendations.
In-Vitro Maturation (IVM) is an innovative approach to assisted reproductive technology that offers an alternative to traditional in-vitro fertilization (IVF). By retrieving and maturing immature eggs in the laboratory, IVM eliminates or reduces the need for ovarian stimulation and offers potential benefits in terms of cost, time efficiency, and ethical considerations. However, IVM may have lower success rates than traditional IVF, and its availability may have limitations. Deciding on the most appropriate treatment option requires careful consideration and consultation with a fertility specialist. By understanding the concept and potential benefits and limitations of IVM, individuals and couples can make informed decisions regarding their fertility journey.
Twins with IVF: Understanding the Process, Benefits, and Considerations

In recent years, in vitro fertilization (IVF) has emerged as a popular solution for couples facing infertility challenges. Among the various aspects associated with IVF, the possibility of conceiving twins has gained considerable attention. This comprehensive article aims to provide a detailed understanding of twins with IVF, including the process involved, the benefits, and important considerations for couples considering this path to parenthood.
What is IVF?
IVF is a fertility treatment that involves several steps. It begins with hormone stimulation and the administration of fertility medications to stimulate the ovaries. Eggs are then retrieved and fertilized in a laboratory. The resulting embryos are monitored and, after a few days, one or more are transferred to the woman’s uterus.
Understanding Twin Pregnancy:
There are two types of twins: identical and fraternal. Identical twins occur when a single fertilized egg splits into two embryos, while fraternal twins result from the simultaneous fertilization of two separate eggs. Various factors influence the likelihood of conceiving twins, including genetics, family history, and maternal age.
Twins and IVF:
IVF increases the chances of conceiving twins compared to natural conception. By stimulating the ovaries to produce multiple eggs, IVF enhances the probability of fertilization and implantation of multiple embryos. While having twins can be seen as advantageous in some cases, there are also potential drawbacks and increases in risks associated with multiple pregnancies.
Benefits of Twins with IVF:
For couples struggling with infertility, the possibility of conceiving twins can bring emotional and psychological benefits. It may offer a sense of fulfillment and completeness in their journey to parenthood. Additionally, having twins can provide financial advantages, as it reduces the need for future IVF cycles. Furthermore, twin parents often benefit from a supportive community and resources specifically tailored to their unique needs.
Important Considerations:
Couples considering twins with IVF should consult with fertility specialists to thoroughly evaluate their specific circumstances. Factors such as individual health, pregnancy risks, emotional preparedness, and the impact on existing children and family dynamics must be carefully considered. Understanding the potential challenges associated with raising twins is crucial for making informed decisions.
Managing a Twin Pregnancy:
Prenatal care plays a vital role in the well-being of both the mother and the twins. Regular monitoring, proper nutrition, and weight gain are essential during pregnancy. Twins are at a higher risk of certain complications, so preventive measures and additional medical attention are necessary. Building a support system and accessing twin-specific resources can greatly assist parents throughout the journey.
Postnatal Considerations:
Raising twins comes with its own set of challenges and joys. Balancing the individual needs and attention for each child is crucial. Implementing effective parenting strategies specific to twins can help foster their development. Additionally, seeking support networks and guidance from experienced twin parents can provide valuable assistance in navigating the unique aspects of raising twins.
As the demand for fertility treatments like IVF continues to rise, understanding the possibility of conceiving twins is crucial for couples considering this path. While twins can bring immense joy and benefits, it is important to approach this journey with awareness and preparation. By comprehending the process, benefits, and considerations associated with twins through IVF, couples can make informed decisions, seek appropriate medical guidance, and embrace the challenges and rewards of raising twins. Consulting with fertility specialists, understanding individual health factors, and preparing emotionally are key to ensuring the best possible outcomes for both parents and their future children.
The Egg Retrieval Process: Everything you need to know

If you are considering egg retrieval as a part of your fertility treatment journey or are simply curious about the process, this comprehensive guide will provide you with all the essential information you need to know. From understanding the procedure to preparing for it and the potential risks and benefits, let’s delve into the world of egg retrieval.
What is Egg Retrieval?
Egg retrieval, also known as oocyte retrieval, is a crucial step in the in vitro fertilization (IVF) process. During this procedure, eggs are retrieved from a woman’s ovaries to be fertilized in a laboratory setting. The collected eggs are then combined with sperm to facilitate fertilization, ultimately aiming to create embryos that can be transferred into the woman’s uterus.
Understanding the Procedure
Egg retrieval is typically performed under sedation or anesthesia to minimize discomfort. Using an ultrasound-guided probe, a fertility specialist will gently aspirate the follicles in the ovaries to retrieve the eggs. The entire process usually takes around 20-30 minutes.
Before the procedure, your doctor may prescribe hormonal medications to stimulate the growth and maturation of multiple eggs. These medications help increase the chances of retrieving a sufficient number of healthy eggs for successful fertilization.
Preparing for Egg Retrieval
Preparing for egg retrieval involves a series of steps to ensure optimal results. Here are some essential aspects to consider:
1. Consultation: Schedule a consultation with a fertility specialist who will assess your medical history, perform necessary tests, and discuss the entire process, including potential risks and complications.
2. Medication Regimen: Your doctor will prescribe hormonal medications to stimulate egg production. It is crucial to follow the medication regimen precisely as prescribed.
3. Lifestyle Modifications: Making certain lifestyle modifications can contribute to the success of egg retrieval. Quitting smoking, reducing alcohol intake, and maintaining a healthy diet and exercise routine can positively impact your fertility.
4. Emotional Support: Egg retrieval can be emotionally taxing, so it’s important to build a strong support system. Seek support from your partner, family, friends, or even consider joining support groups or counseling sessions.
Potential Risks and Complications
While egg retrieval is generally considered a safe procedure, it is important to be aware of potential risks and complications. Some of the common risks include:
1. Infection: There is a slight risk of infection after the procedure. Your doctor will prescribe antibiotics to minimize this risk.
2. Ovarian Hyperstimulation Syndrome (OHSS): OHSS is a condition where the ovaries become swollen and painful due to an excessive response to fertility medications. This can be managed through proper monitoring and medication adjustments.
3. Bleeding or Injury: Rarely, there may be a risk of bleeding or injury to blood vessels or organs during the procedure. However, the risk is minimized with the use of ultrasound guidance.
Benefits of Egg Retrieval
Egg retrieval offers several benefits, particularly for couples struggling with infertility. Some of these benefits include:
1. Increased Pregnancy Success Rates: By combining retrieved eggs with sperm in a controlled laboratory environment, the chances of successful fertilization and subsequent pregnancy are significantly improved.
2. Genetic Testing: Eggs obtained through retrieval can undergo genetic testing, allowing for the selection of healthy embryos and reducing the risk of passing on genetic disorders.
3. Cryopreservation: Excess eggs obtained during retrieval can be cryopreserved, allowing individuals or couples to use them at a later time, even after the initial IVF cycle.
4. Donor Egg Options: Egg retrieval opens the possibility of using donor eggs, which can be a viable option for individuals or couples who are unable to use their own eggs.
Egg retrieval is a crucial step in the IVF process, offering hope for couples struggling with infertility. By understanding the procedure, preparing adequately, and being aware of potential risks and benefits, individuals can make informed decisions and embark on their fertility treatment journey with confidence. Remember, consulting with a fertility specialist and building a strong support system can greatly contribute to the overall success and well-being throughout the process.
Optimizing IVF Success with Neupogen

In the realm of assisted reproductive technology, couples grappling with infertility are increasingly exploring innovative avenues to enhance their chances of success with in vitro fertilization (IVF). Among these possibilities, the integration of Neupogen, a medication traditionally utilized in cancer treatments, into the IVF protocol has garnered attention. This comprehensive guide seeks to unravel the intricacies of Neupogen IVF, shedding light on its role, success rates, benefits, and the protocol involved in this cutting-edge fertility treatment. Additionally, we will delve into the potential side effects.
Understanding Neupogen and its Role in IVF:
Neupogen, also known as Filgrastim, is a synthetic form of granulocyte-colony stimulating factor (G-CSF), a protein naturally occurring in the body. Originally designed to stimulate the production of white blood cells in cancer patients undergoing chemotherapy, Neupogen has shown promise in the realm of reproductive medicine, particularly in the context of in vitro fertilization (IVF).
In the intricate dance of IVF, successful embryo implantation is crucial for a positive outcome. Neupogen is believed to play a pivotal role in this process by enhancing the receptivity of the uterine lining. A receptive uterine environment is essential for the embryo to successfully implant and develop into a pregnancy. Neupogen is thought to promote this receptivity by influencing the endometrial lining, making it more conducive for embryo attachment.
Moreover, Neupogen’s potential immunomodulatory effects are noteworthy. It is suggested to modulate the immune response in a way that reduces the risk of implantation failure, particularly in cases where the immune system may be overly active, hindering the embryo’s successful attachment.
The ability of Neupogen to address challenges such as thin endometrial lining or immune-related factors positions it as a promising addition to the IVF toolkit. As researchers continue to delve into the specific mechanisms and intricacies of Neupogen’s role in IVF, its application is becoming increasingly tailored to individual patient needs, offering a beacon of hope for couples navigating the complexities of infertility.
Benefits of Neupogen in IVF:
While Neupogen has been primarily associated with its potential to improve IVF success rates, several benefits are noteworthy:
-
Improved Endometrial Receptivity:
Neupogen has been reported to enhance endometrial receptivity, creating an environment conducive to successful embryo implantation. This benefit is particularly relevant for individuals with a history of thin endometrial lining, a common challenge in infertility cases.
-
Potential Immune Modulation:
Neupogen may contribute to immune modulation, reducing the risk of implantation failure associated with immunological factors. This benefit is particularly significant for individuals with a history of recurrent implantation failure or immune-related fertility challenges.
-
Increased Implantation Rates:
Studies and clinical trials have suggested that Neupogen use in IVF protocols is associated with increased implantation rates. Improved implantation rates contribute directly to higher overall pregnancy success.
-
Enhanced Ovarian Stimulation Response:
Neupogen may positively impact ovarian stimulation response, leading to a more robust development of eggs during the IVF cycle. This benefit is particularly relevant for individuals who have experienced suboptimal ovarian responses in previous IVF cycles.
Neupogen IVF Success Stories:
Numerous success stories have emerged from couples who have incorporated Neupogen into their IVF protocols. While individual experiences may vary, several studies and clinical trials have reported positive outcomes, including increased implantation rates and higher overall pregnancy success.
Researchers attribute the success of Neupogen in IVF to its ability to address underlying issues such as a thin endometrial lining or immune-related factors that may hinder embryo implantation. By providing a conducive uterine environment, Neupogen aims to tip the odds in favor of a successful pregnancy.
Neupogen IVF Protocol:
Implementing Neupogen into the IVF protocol requires a strategic and personalized approach. Below is a detailed breakdown of the protocol:
-
Patient Assessment and Selection:
– Before incorporating Neupogen, a thorough assessment of the patient’s medical history and fertility challenges is essential.
– Factors such as age, previous IVF failures, and uterine conditions are considered to identify candidates who may benefit from Neupogen.
-
Timing and Dosage:
– Neupogen is typically administered during the ovarian stimulation phase of the IVF cycle.
– The dosage and frequency are tailored to the individual’s specific needs, considering factors such as ovarian response and underlying fertility challenges.
-
Administration Route:
– Neupogen can be administered via intravenous (IV) infusion or subcutaneous injection.
– The chosen route depends on the patient’s medical history, preferences, and the treating physician’s recommendation.
-
Monitoring and Adjustments:
– Ongoing monitoring of the patient’s response to Neupogen is crucial throughout the IVF cycle.
– Adjustments to the dosage or administration schedule may be made based on the individual’s progress and the treatment plan’s effectiveness.
-
Combination with Standard IVF Protocols:
– Neupogen is often integrated into existing IVF protocols, complementing standard procedures such as ovarian stimulation, egg retrieval, and embryo transfer.
Side Effects of Neupogen in IVF:
While Neupogen is generally well-tolerated, it is crucial to be aware of potential side effects associated with its use in the context of IVF:
-
Bone Pain:
Neupogen use has been linked to bone pain, particularly in the pelvis and long bones. Patients are encouraged to communicate any discomfort to their healthcare provider, who may consider adjusting the dosage or recommend pain management strategies.
-
Flu-Like Symptoms:
Some individuals may experience flu-like symptoms, including fever, chills, and muscle aches, as a result of Neupogen administration. These symptoms are typically temporary and tend to resolve on their own. However, patients are advised to inform their healthcare team if symptoms persist.
-
Headache and Fatigue:
Neupogen use may be associated with headaches and fatigue in some cases. Adequate rest and hydration can help alleviate these symptoms, but patients should report persistent or severe effects to their healthcare provider.
-
Allergic Reactions:
While rare, allergic reactions to Neupogen may occur, presenting as rash, itching, swelling, severe dizziness, or difficulty breathing. In the event of any allergic reaction, immediate medical attention is crucial.
Considerations and Consultation:
Before embarking on the Neupogen IVF journey, several considerations merit attention:
Patient-Specific Assessment:
– Comprehensive evaluation of the patient’s medical history, fertility challenges, and previous IVF experiences.
– Identification of individuals who may benefit from Neupogen based on factors like age, uterine conditions, and prior IVF failures.
Shared Decision-Making:
– In-depth discussions between the patient and healthcare provider about the potential benefits and risks of Neupogen.
– Shared decision-making, ensuring that the choice to incorporate Neupogen aligns with the patient’s goals and values.
Individualized Treatment Plan:
– Tailoring the Neupogen IVF protocol to the individual’s specific needs, adjusting dosage and administration routes accordingly.
– Integration with standard IVF procedures to create a holistic and personalized treatment plan.
Ongoing Monitoring and Adaptations:
– Regular monitoring of the patient’s response to Neupogen throughout the IVF cycle.
– Adaptations to the protocol based on the individual’s progress, ensuring optimal effectiveness.
Potential Alternative Approaches:
– Consideration of alternative approaches or complementary treatments based on the patient’s profile and response to Neupogen.
– Flexibility to adapt the treatment plan as needed for the best possible outcome.
Conclusion:
In conclusion, the integration of Neupogen into IVF protocols represents a promising frontier in the field of assisted reproductive technology. The multifaceted benefits of Neupogen, ranging from improved endometrial receptivity to potential immune modulation, have captured the attention of both clinicians and hopeful parents-to-be.
The success stories of couples who have incorporated Neupogen into their IVF journeys, coupled with positive outcomes reported in studies and clinical trials, underscore the potential of this innovative approach. Neupogen’s ability to address specific challenges, such as thin endometrial lining or immune-related factors, positions it as a valuable tool in enhancing IVF success rates.
However, as with any medical intervention, it is crucial to approach Neupogen use in IVF with a comprehensive understanding of its benefits and potential side effects. The decision to integrate Neupogen into an IVF protocol should be made collaboratively between patients and their healthcare providers, considering individualized needs and the latest scientific evidence.
Ongoing research will continue to illuminate the nuances of Neupogen’s role in fertility treatments, further refining its application and expanding the possibilities for those on their journey toward parenthood. As Neupogen gains recognition and becomes a more integral part of IVF protocols, the potential for improved success rates and fulfilling the dreams of parenthood stands as a beacon of optimism for the future of assisted reproduction.
IVF for Men: A Comprehensive Guide to Understanding the Process and Your Role

Welcome to our comprehensive guide on IVF (in vitro fertilization) for men. In this article, we will delve into the intricacies of the IVF process and provide valuable insights for men who are embarking on this journey. From understanding the basics of IVF to exploring the role you play, we aim to equip you with the knowledge and understanding necessary to navigate your way through the IVF process.
Understanding IVF
IVF is a fertility treatment that involves the fertilization of eggs outside the body. It begins with the stimulation of the female partner’s ovaries to produce multiple eggs. These eggs are then retrieved and combined with sperm in a laboratory setting. After fertilization, the resulting embryos are carefully monitored, and one or more are transferred into the female partner’s uterus in the hopes of achieving a successful pregnancy.
Your Role in the IVF Process
As a man, your role is crucial in the IVF process. Here are the key aspects for you to consider:
1. Sperm Analysis: Your fertility specialist will conduct a comprehensive analysis of your sperm, including assessing its count, motility, and morphology. This analysis provides crucial information regarding your sperm’s ability to fertilize an egg.
2. Providing a Semen Sample: During the IVF process, you will be required to provide a semen sample. This sample will be used in the laboratory to fertilize the retrieved eggs. It is important to follow the guidelines provided by the fertility clinic for collecting and delivering the sample.
3. Supporting Your Partner: Going through IVF for men can be emotionally and physically demanding for both partners. Providing emotional support, attending appointments together, and engaging in open and honest communication can strengthen your relationship and help navigate the IVF journey effectively.
4. Lifestyle Factors: Lifestyle choices can impact fertility. Prioritize maintaining a healthy lifestyle by eating a balanced diet, exercising regularly, managing stress, and avoiding harmful habits such as smoking or excessive alcohol consumption. These factors contribute to overall sperm health and can positively influence the success of IVF.
Addressing Common Concerns and Questions
1. Is IVF a Safe Procedure?
IVF is a safe procedure, with millions of successful births worldwide. However, like any medical intervention, it carries certain risks, such as the potential for infections, multiple pregnancies, or ovarian hyperstimulation syndrome (OHSS). It is important to discuss these risks with your healthcare provider to have a clear understanding of what to expect.
2. What Can Impact Male Fertility?
Various factors can affect male fertility, including age, genetics, underlying medical conditions, lifestyle choices, and environmental factors. It is essential to undergo a thorough fertility evaluation to assess any potential underlying issues.
3. Can Lifestyle Changes Improve Fertility?
Adopting a healthy lifestyle can positively impact fertility. Maintaining a balanced diet, engaging in regular physical activity, managing stress levels, avoiding excessive heat exposure to the testicles, and eliminating harmful habits can potentially improve sperm quality and overall fertility.
4. What Emotional Challenges May Arise?
The IVF process can often be emotionally challenging for both partners. Feelings of stress, anxiety, and grief are common. Open communication, seeking emotional support, and exploring coping mechanisms such as counseling or support groups can be beneficial in navigating these challenges.
As a man going through the IVF process, understanding your role and actively participating is crucial. By familiarizing yourself with the basics of IVF, providing a semen sample, supporting your partner, and prioritizing a healthy lifestyle, you can contribute to the success of the IVF journey. Remember, open communication and seeking professional guidance are key to a smoother and more effective IVF experience.
